What Is COPD, Really?
COPD isn’t just a bad cough or wheezing when you climb stairs. It’s a serious, long-term lung disease that makes it harder and harder to breathe. The name stands for Chronic Obstructive Pulmonary Disease, and it’s not one single illness-it’s mostly two: chronic bronchitis and emphysema. Both damage your airways and air sacs, so less oxygen gets into your blood and carbon dioxide builds up. Most people get it from smoking. In fact, 85 to 90% of cases are linked to cigarettes. But it’s not just smokers-long-term exposure to fumes, dust, or pollution can also cause it. The damage is permanent, but it doesn’t have to control your life.
How COPD Gets Worse: The Four Stages
COPD doesn’t hit all at once. It creeps in slowly. Doctors use a test called spirometry to measure how much air you can force out of your lungs in one second-called FEV1. This number tells them how far the disease has gone. There are four clear stages, and knowing which one you’re in helps guide treatment.
Stage 1: Mild COPD means your FEV1 is 80% or higher of what’s normal for someone your age and size. You might have a daily cough with mucus, and you get winded after running or lifting heavy stuff. But most people blame it on getting older or being out of shape. That’s why nearly half of people with Stage 1 COPD don’t get diagnosed for years. The good news? Catching it here gives you the best shot at slowing it down.
Stage 2: Moderate COPD shows up when FEV1 drops to 50-79%. Now, you’re short of breath just walking on flat ground. You might stop every few minutes to catch your breath. Daily tasks like getting dressed or making a meal become harder. This is the stage where most people finally go to the doctor. By now, lung function has dropped enough that you can’t ignore it.
Stage 3: Severe COPD means your FEV1 is between 30-49%. Breathing becomes a constant struggle. You can’t walk more than a few steps without stopping. You might need help with showering or cooking. Flare-ups-called exacerbations-are common, happening three or more times a year. These can land you in the hospital and speed up lung damage.
Stage 4: Very Severe (End-Stage) COPD is when FEV1 falls below 30%, or below 50% with chronic low oxygen. You’re breathless even at rest. Simple things like talking or brushing your teeth leave you gasping. Many need oxygen 24 hours a day. Some develop blue lips or fingernails from lack of oxygen. Confusion and weight loss are common. This stage carries the highest risk of sudden, life-threatening flare-ups.
How Doctors Decide What Treatment You Need
It’s not just about your FEV1 anymore. The latest guidelines (GOLD 2023) look at two big things: how much your symptoms bother you, and how often you have flare-ups. That’s why patients are grouped into A, B, C, or D-not just 1, 2, 3, 4. Group A has few symptoms and rare flare-ups. Group D has lots of symptoms and frequent flare-ups. Your group shapes your treatment plan.
Treatment by Stage: What Actually Works
Stage 1: Quit Smoking-Now This is the single most powerful thing you can do. Quitting can cut the rate of lung decline by half. No other treatment comes close. Short-acting inhalers like albuterol can help if you’re winded during exercise, but they’re not daily medicine yet.
Stage 2: Add Long-Acting Inhalers You’ll likely start on a long-acting bronchodilator-either tiotropium (Spiriva) or salmeterol (Serevent). These open your airways for 12 to 24 hours. You’ll also be asked to join pulmonary rehab. It’s not just exercise-it’s education, breathing techniques, and support. Studies show it helps people walk 54 meters farther in six minutes. Get your flu shot every year. Pneumonia shots too. These prevent flare-ups that can wreck your lungs.
Stage 3: Combination Therapy You’ll probably use two long-acting inhalers together: a LAMA and a LABA. If you’re having frequent flare-ups, your doctor may add an inhaled steroid. Oxygen might be needed if your blood oxygen drops below 88% at rest. Many patients here start needing help with daily tasks. Pulmonary rehab is even more critical-it cuts hospital visits by 37%.
Stage 4: Oxygen and Big Decisions Continuous oxygen therapy (15+ hours a day) can extend life by 44% if you’re severely low on oxygen. Portable oxygen tanks help, but they only last 4-6 hours at standard flow. Many patients feel trapped by the tubing. For some, lung volume reduction surgery helps remove damaged parts of the lung so the rest can work better. Lung transplant is an option for people under 65 with FEV1 under 20% and no other major health issues. It’s not a cure, but it can give you years of better breathing.
What No One Tells You About COPD Treatment
Most people think taking an inhaler is enough. It’s not. Up to 80% of patients use their inhalers wrong. You need someone to watch you-three or four times-until you get it right. A puff without holding your breath? It’s wasted. A mist going into your eyes? You’re not getting the medicine.
Cost is another hidden barrier. Spiriva costs $350-$400 a month without insurance. Oxygen equipment is covered by Medicare, but the deductible is $233, and portable units are heavy and loud. Many patients avoid going out because they can’t carry their oxygen far enough.
And then there’s adherence. Half of people stop taking their meds within six months. Why? Side effects, confusion, cost, or just feeling fine one day and thinking they don’t need it. But COPD doesn’t wait. Skipping doses speeds up decline.

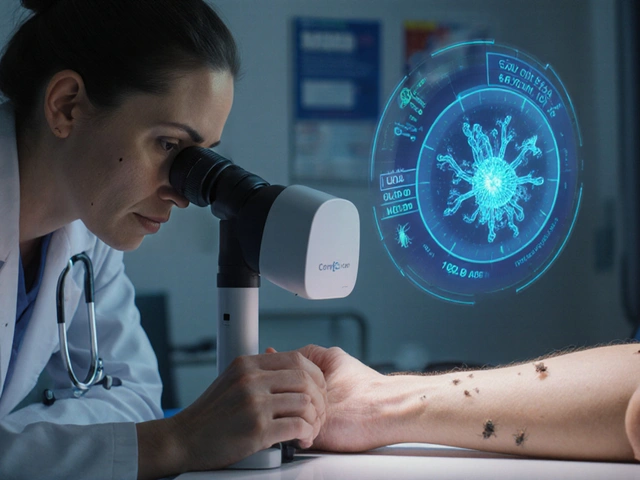
New Hope on the Horizon
There’s progress. In 2023, the FDA approved Breztri Aerosphere-the first single inhaler that combines three medications (LAMA, LABA, and steroid). It’s simpler than juggling three separate devices. A new drug called ensifentrine, still in trials, improved lung function by 13% in early tests. There’s also AI-powered apps like Kyna COPD that track your symptoms and predict flare-ups with 82% accuracy. That means you can act before you’re gasping.
Genetic research is growing too. The NIH’s COPDGene study found 82 gene variants linked to how fast COPD worsens. In the future, treatment might be tailored to your DNA, not just your FEV1.
What You Can Do Today
Even if you’re in Stage 4, you’re not powerless. Pulmonary rehab works at every stage. Nutrition matters-many COPD patients lose weight because breathing burns so many calories. Eating enough protein and calories helps you keep strength. Stay up to date on vaccines. Avoid smoke, dust, and cold air. Learn the warning signs of a flare-up: more cough, thicker mucus, increased shortness of breath, or swelling in your ankles. Act fast-call your doctor at the first sign.
Connect with others. The COPD Foundation has over 100 local support groups and 25,000 active online members. You’re not alone. People who join support groups report better moods, better adherence to meds, and fewer hospital stays.
Final Thoughts: It’s Not a Death Sentence
COPD is serious. It’s the third leading cause of death worldwide. But it’s not a race to the end. Many people live for years-decades-with good quality of life. The key is early detection, consistent treatment, and not giving up. Quitting smoking at any stage helps. Taking your meds right helps. Getting rehab helps. Using oxygen correctly helps. You don’t need to be perfect. You just need to keep moving forward, one breath at a time.
Can COPD be cured?
No, COPD cannot be cured. The lung damage is permanent. But it can be managed effectively. Stopping smoking, using prescribed medications correctly, doing pulmonary rehab, and avoiding triggers can slow progression, reduce flare-ups, and help you live well for many years.
How is COPD diagnosed?
COPD is diagnosed with a simple breathing test called spirometry. You blow into a tube as hard and fast as you can. The machine measures how much air you can force out in one second (FEV1) and how much total air you can exhale (FVC). If your FEV1/FVC ratio is low, and it doesn’t improve much with a bronchodilator, COPD is likely. Your doctor will also ask about your smoking history, symptoms, and exposure to lung irritants.
What’s the difference between asthma and COPD?
Asthma usually starts in childhood and causes reversible airway narrowing-meaning your lungs bounce back after a flare-up. COPD is progressive, caused mostly by smoking, and the damage is permanent. Asthma symptoms often come and go quickly; COPD symptoms get worse slowly over time. Some people have both-called asthma-COPD overlap syndrome (ACOS)-and need special treatment.
Can I still exercise with COPD?
Yes-and you should. Exercise strengthens your muscles, including the ones you use to breathe. You won’t be able to run marathons, but walking, cycling on a stationary bike, or doing light strength training can make a big difference. Pulmonary rehab programs are designed for COPD patients and teach you how to exercise safely without overdoing it.
How do I know if I’m having a COPD flare-up?
Watch for three key signs: more shortness of breath than usual, increased cough or wheezing, and changes in your mucus-like more volume, thicker texture, or a darker color (yellow or green). You might also feel more tired, have swollen ankles, or find your inhaler isn’t helping like it used to. Call your doctor at the first sign. Early treatment can stop a flare-up from becoming a hospital trip.
Is oxygen therapy addictive?
No, oxygen is not addictive. Your body needs oxygen to live. If your lungs can’t get enough into your blood, supplemental oxygen is just replacing what’s missing. It doesn’t change your lungs’ ability to work. In fact, long-term oxygen therapy can improve your survival and quality of life if you have severe low oxygen levels.
What’s the life expectancy with COPD?
There’s no single answer-it depends on your stage, whether you smoke, your age, other health problems, and how well you follow your treatment plan. Someone with mild COPD who quits smoking can live for decades. Someone with severe COPD and frequent flare-ups may have a shorter life expectancy, but even then, proper care can add years. The goal isn’t just to live longer-it’s to live better, with more energy and fewer hospital visits.





Connor Moizer
November 17, 2025 AT 20:56Man, I wish I’d read this five years ago. I kept telling myself it was just ‘smoker’s cough’-until I couldn’t climb two flights without stopping. Now I’m Stage 3, on oxygen 18 hours a day, and I still mess up my inhaler. The part about 80% of people using them wrong? Yeah. That’s me. I’ve wasted so much money on meds that just flew out of my mouth. But I’m learning. Pulmonary rehab saved my life. Not because it’s magic-it’s because they actually watched me breathe. No one else ever did.
kanishetti anusha
November 18, 2025 AT 16:35Thank you for writing this. I’m from India, and my dad has COPD. No one here talks about it like this. Doctors just hand out inhalers and say ‘stop smoking.’ But we don’t have access to rehab, or even clean air. My mom burns cow dung for cooking-that’s his trigger. I’m trying to get him a portable oxygen concentrator, but it costs more than our monthly rent. This post made me feel less alone. We’re not just numbers in a chart.
roy bradfield
November 19, 2025 AT 22:23Let me tell you what they don’t want you to know. COPD isn’t caused by smoking. It’s caused by Big Pharma. They made the inhalers expensive so you’d keep buying them. The real cause? Fluoride in the water. They’ve been poisoning our lungs since the 50s to sell more oxygen tanks. Look at the data-cities with fluoridated water have 3x the COPD rates. And why is Breztri so expensive? Because they’re keeping the three-drug combo patent locked down. They don’t want you to get better-they want you dependent. The government knows. The WHO knows. But they won’t tell you. That’s why you’re still breathing like a broken bellows.
Patrick Merk
November 21, 2025 AT 02:24Brilliant breakdown. I’ve been a respiratory therapist for 18 years, and this is the clearest summary I’ve seen in a decade. The part about Group A-D classification? So many docs still treat by FEV1 alone. It’s like judging a car’s performance only by its engine size, ignoring the tires, the suspension, and whether the driver’s asleep. Pulmonary rehab is the unsung hero here. It’s not glamorous, but it’s the only thing that consistently improves quality of life across all stages. And yes-yes-yes to the inhaler technique. I’ve watched grown men cry because they realized they’d been wasting $400 a month on mist.
Liam Dunne
November 22, 2025 AT 11:35Just got diagnosed Stage 2 last month. Quit smoking yesterday. Took me 27 years. I’m not gonna lie-it’s the hardest thing I’ve ever done. But I’m doing rehab next week. I’m scared, but I’m doing it. Also, I just bought a $20 spacer from Amazon. My inhaler finally works now. Thanks for the heads-up about the cost. I was about to skip the pneumonia shot because I thought it was ‘optional.’ Not anymore.
Vera Wayne
November 23, 2025 AT 22:51Thank you, thank you, thank you-for writing this with such clarity, compassion, and accuracy. I’ve spent years watching my mother struggle with Stage 4 COPD, and this post captures everything we’ve lived through-the isolation, the fear, the frustration with the system, the quiet courage it takes to just breathe through another day. Please keep sharing this. People need to know: it’s not about ‘toughing it out.’ It’s about smart, consistent, kind care. And you’re right-it’s not a death sentence. It’s a call to live better, even when it’s hard.
Rodney Keats
November 25, 2025 AT 22:34So let me get this straight-you’re telling me I have to pay $400 a month for a puff that I don’t even know how to use, and if I don’t, I’ll die? Cool. Thanks for the guilt trip. I’m just gonna keep smoking and enjoy my last few years. At least I’ll be happy while I’m dying. You people with your rehab and oxygen tanks and ‘one breath at a time’-you’re just making people feel bad for not being perfect. I’m not a patient. I’m a human. And I’m tired.
Laura-Jade Vaughan
November 26, 2025 AT 08:57OMG I’m crying 😭 this is so beautiful. I just got diagnosed and I was so scared, but now I feel like I can actually DO something. Also, Breztri looks so sleek-like a designer inhaler?? 💫 I’m gonna get one as soon as insurance clears. And oxygen tanks? I’m getting the pink one. Why not? Life’s too short for beige. 🌸 #COPDWarrior #OxygenIsTheNewChic
Jennifer Stephenson
November 26, 2025 AT 23:56Smoking causes COPD. Quitting helps. Inhalers must be used correctly. Rehab improves function. Oxygen extends life. Vaccines prevent flare-ups. These are facts.
Segun Kareem
November 27, 2025 AT 20:06There is a rhythm to breath. When you lose it, you lose more than air-you lose time, connection, dignity. But even in the deepest gasp, the body remembers how to heal. Not magically. Not quickly. But with patience, with community, with small acts of stubborn care. You don’t need to be cured to be whole. You just need to keep showing up. One breath. Then another. That is the quiet rebellion against despair.
Philip Rindom
November 28, 2025 AT 06:13Man, I used to be that guy who rolled his eyes at pulmonary rehab. Thought it was just fancy walking. Then my uncle did it-and he went from barely making it to the fridge to walking his granddaughter to the bus stop. I’m not saying it’s easy. But it’s worth it. And hey, if you’re struggling with meds, just text your doc. No shame. We’ve all been there.
Jess Redfearn
November 28, 2025 AT 23:07Wait so if I stop smoking now, will my lungs grow back? Like, can I just quit and be fine? I don’t wanna do rehab or buy oxygen. Can’t I just take a pill?