When your kidneys start acting up-swelling, fatigue, less urine, or just feeling off-it’s easy to blame a bad night’s sleep or a stomach bug. But if you’ve been taking common medications like omeprazole, ibuprofen, or an antibiotic for weeks or months, something more serious could be happening: acute interstitial nephritis. It’s not a household name, but it’s one of the most common causes of sudden kidney failure in people who aren’t diabetic or hypertensive. And the worst part? It often flies under the radar until it’s too late.
What Exactly Is Acute Interstitial Nephritis?
Acute interstitial nephritis (AIN) is inflammation in the spaces between the kidney’s tubules. These tubules are the tiny filters that clean your blood and make urine. When they get swollen and clogged with immune cells, your kidneys can’t work properly. The result? A sudden drop in kidney function-sometimes so severe you need dialysis.
This isn’t a random glitch. In 60 to 70% of cases, it’s triggered by drugs. Over 250 medications have been linked to AIN, but just a few are behind most cases. The biggest culprits today? Proton pump inhibitors (PPIs) like omeprazole and pantoprazole, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, and certain antibiotics like penicillin and ciprofloxacin.
What’s changed in the last decade? PPIs have overtaken antibiotics as the #1 trigger. Why? Because they’re everywhere-taken daily for heartburn, reflux, or even just "for safety." But what seems like harmless long-term use can quietly damage your kidneys. Studies now show 12 out of every 100,000 people develop AIN from PPIs each year. That’s not rare. It’s a growing public health issue.
How Do Drugs Actually Damage the Kidneys?
It’s not about toxicity. Most of these drugs aren’t poisons. Instead, they trigger an immune reaction. Your body mistakes part of the drug-or a molecule it creates-as a threat. White blood cells swarm into the kidney tissue, causing inflammation. Eosinophils (a type of immune cell) show up, tubules get damaged, and fluid builds up. This is called a hypersensitivity reaction.
Here’s the twist: the classic signs-rash, fever, and eosinophilia (high eosinophil count in blood)-only show up in fewer than 10% of cases. Most people don’t get a rash. They just feel tired, lose their appetite, or notice their urine is darker. Some develop mild joint pain or a low-grade fever. These symptoms are so vague, they’re often mistaken for a virus or a urinary tract infection.
And the timing? It varies wildly. Antibiotics can cause AIN within days. NSAIDs? Often after months or even years of use. PPIs? Typically after 6 to 18 months. That’s why doctors rarely connect the dots. A 65-year-old on omeprazole for three years might be told their rising creatinine is just "aging." But it’s not aging. It’s AIN.
Which Drugs Are the Biggest Risks?
Not all drug-induced AIN is the same. The type of drug affects how bad it gets-and whether your kidneys recover.
- NSAIDs (44% of drug-induced cases): These cause the most chronic damage. Patients often have proteinuria (protein in urine) at levels seen in nephrotic syndrome. Recovery is slower and less complete. About 42% develop permanent kidney damage.
- Antibiotics (33% of cases): These tend to come on fast-within 10 days. They’re more likely to cause the classic hypersensitivity signs, but they also have the best recovery rate. Around 70-80% of patients regain full kidney function if caught early.
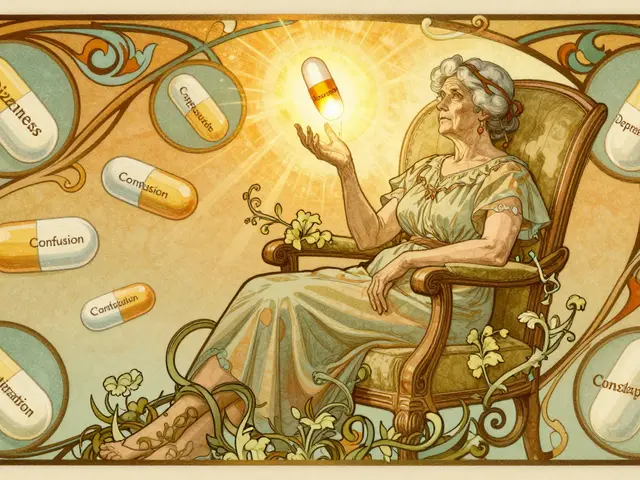
- PPIs (29-38% of cases): These cause less dramatic symptoms, which makes them dangerous. People don’t realize they’re sick until their eGFR (kidney function number) drops below 45. Recovery is poor: only 50-60% get back to normal. Many are left with stage 3 chronic kidney disease.
Even more concerning: the risk jumps with age and polypharmacy. If you’re over 65 and taking five or more medications, your risk is more than three times higher than someone on just one or two. That’s why older adults on heart meds, blood pressure pills, and daily PPIs are the most vulnerable group.

How Is It Diagnosed?
There’s no simple blood test. No single lab value confirms AIN. Creatinine and BUN might rise, but so do they in dehydration or other kidney problems. Urine tests might show white blood cells or eosinophils-but eosinophiluria is only present in about half the cases.
The only definitive way to diagnose AIN is a kidney biopsy. Yes, it’s invasive. But it’s necessary. Without it, you might be misdiagnosed with glomerulonephritis, acute tubular necrosis, or just "unexplained kidney failure."
Biopsy findings show immune cells flooding the space between tubules, swollen tissue, and sometimes early scarring. If you’re on a PPI and your biopsy shows this pattern, the diagnosis is clear. And that’s when treatment needs to start-immediately.
Recovery: What Actually Happens After Stopping the Drug?
The single most important step? Stop the drug. That’s it. No fancy treatment. No miracle cure. Just removal of the trigger.
Studies show that 65% of patients notice improvement within 72 hours of stopping the offending medication. Urine output increases. Fatigue lifts. Creatinine starts to fall. But recovery speed depends on the drug:
- Antibiotic-induced: median recovery in 14 days
- NSAID-induced: median recovery in 28 days
- PPI-induced: median recovery in 35 days
But here’s the hard truth: stopping the drug doesn’t guarantee full recovery. About 30% of patients develop chronic kidney disease within a year. That means their eGFR stays below 60 mL/min/1.73m² permanently. NSAID users are most at risk-nearly half never fully bounce back.
One patient case from the American Kidney Fund tells the story: a 63-year-old woman on omeprazole for 18 months developed AIN. Her creatinine spiked. She needed dialysis for three weeks. Even after recovery, her kidney function stayed at eGFR 45-down from 85 before the drug. She’s now on lifelong kidney monitoring.
Do Steroids Help?
This is controversial. There are no large randomized trials proving corticosteroids like prednisone save kidneys in AIN. But doctors use them anyway-especially when kidney function is severely low (eGFR under 30) or not improving after 72 hours of stopping the drug.
The typical protocol? Start with methylprednisolone (0.5-1 mg/kg/day) for 2-4 weeks, then switch to oral prednisone and taper slowly over 6-8 weeks. The European Renal Association supports this approach. Experts like Dr. Ronald J. Falk from UNC Kidney Center say it’s the best shot we have for preventing permanent damage.
But steroids aren’t magic. They don’t reverse scarring. If fibrosis has already started, steroids won’t undo it. That’s why timing matters so much. If you wait two weeks to start treatment, your chance of full recovery drops by 35%.

What Happens If It’s Missed?
Delayed diagnosis is the norm, not the exception. The American Kidney Fund reports patients often wait 2-4 weeks before getting the right diagnosis. Why? Because symptoms mimic infections, dehydration, or even stress.
On Reddit’s r/kidneydisease forum, 87 people shared their AIN stories. Nearly a third were misdiagnosed with UTIs. Many were told to "drink more water" or "take a break from painkillers"-without ever considering AIN. By the time they saw a nephrologist, their kidneys were already scarred.
Long-term, 1 in 3 people with AIN end up with stage 3 or worse chronic kidney disease. That means higher risk of heart disease, stroke, and eventual need for dialysis. And the numbers are climbing. Between 2010 and 2020, drug-induced AIN cases rose 27%, mostly because of PPI overuse.
How to Protect Yourself
You don’t need to avoid all medications. But you do need to be smart.
- If you’re on a PPI for more than a year, ask your doctor if you still need it. Many people take them long after their symptoms are gone.
- Don’t combine NSAIDs with PPIs unless absolutely necessary. The combo increases kidney risk.
- Monitor your kidney function if you’re over 65 or on five or more medications. A simple eGFR blood test every 6-12 months can catch early decline.
- Know the red flags: unexplained fatigue, decreased urine, swelling in ankles, nausea without stomach upset. If you’re on one of these drugs and get these symptoms, get your kidneys checked.
AIN is preventable. It’s treatable-if caught early. But it’s not something you can ignore. Your kidneys don’t scream. They whisper. And if you’re not listening, they’ll stop working.
Can acute interstitial nephritis be reversed completely?
Yes, but only if caught early and the causative drug is stopped immediately. About 70-80% of patients with antibiotic-induced AIN recover full kidney function. For NSAID or PPI-induced cases, recovery is less certain-only 50-60% regain normal function. Permanent damage can occur if inflammation leads to scarring, which is irreversible.
How long does it take to recover from drug-induced AIN?
Recovery time varies by drug. Antibiotic-induced cases often improve within 14 days. NSAID-induced cases take about 28 days. PPI-induced cases can take 35 days or longer. Improvement usually starts within 72 hours of stopping the drug, but full recovery may take weeks to months. Kidney function is typically monitored for 6-12 months after diagnosis.
Are proton pump inhibitors (PPIs) safe for long-term use?
PPIs are effective for short-term use, but long-term use increases the risk of acute interstitial nephritis, bone fractures, and nutrient deficiencies. Studies show 12 cases per 100,000 people per year develop AIN from PPIs. If you’ve been on a PPI for more than a year, talk to your doctor about whether you still need it. Many people can taper off safely.
Do I need a kidney biopsy to diagnose AIN?
Yes. While blood and urine tests can suggest AIN, only a kidney biopsy can confirm it. Other conditions like glomerulonephritis or acute tubular necrosis look similar on labs. A biopsy shows immune cell buildup in the kidney’s interstitial tissue-the hallmark of AIN. It’s the only way to rule out other causes and guide treatment.
Can AIN come back after recovery?
If you restart the same drug that caused AIN, it almost always returns-and faster and worse than before. Even if you recover fully, you should avoid that medication for life. Cross-reactivity is common: if you had AIN from one antibiotic, you may react to others in the same class. Always inform all your doctors about your history of AIN.
Is AIN more common in older adults?
Yes. The risk increases sharply with age. While only 5 out of 100,000 people aged 18-44 develop drug-induced AIN, that number jumps to 22 out of 100,000 for those over 65. Older adults are more likely to be on multiple medications, have reduced kidney function naturally, and take PPIs long-term-all major risk factors.
What are the long-term risks after recovering from AIN?
Even after recovery, about 30% of patients develop chronic kidney disease (stage 3 or higher) within a year. NSAID-induced AIN carries the highest risk-42% progress to chronic kidney disease. Long-term monitoring of kidney function (eGFR and urine protein) is essential. Cardiovascular risk also increases with reduced kidney function, so blood pressure and cholesterol control become even more important.
What Comes Next?
If you’ve been diagnosed with AIN, your next steps are simple but critical:
- Stop the offending drug immediately. Don’t wait for your next appointment.
- Get a kidney biopsy if you haven’t already. Confirm the diagnosis.
- Start monitoring your eGFR every 2-4 weeks until stable, then every 3-6 months.
- Avoid NSAIDs and PPIs for life. Use alternatives like H2 blockers (famotidine) for heartburn if needed.
- Inform all future doctors about your history. Add it to your medical record.
If you’re not diagnosed yet but take these drugs daily and feel off-don’t wait. Ask for a kidney function test. A simple creatinine and eGFR blood test takes five minutes. It could save your kidneys.





Evelyn Salazar Garcia
November 30, 2025 AT 09:43Just stopped my omeprazole after reading this. No more magic pills for heartburn. My kidneys aren't a sacrifice zone.
Clay Johnson
December 2, 2025 AT 08:29The immune-mediated mechanism of AIN is a textbook example of molecular mimicry gone awry. Drug antigens bind to tubular basement membranes, triggering T-cell infiltration. No toxicity required. Just misrecognition. The real tragedy is systemic medical inertia.
Jermaine Jordan
December 3, 2025 AT 17:35This isn't just medical advice-it's a wake-up call for an entire generation addicted to quick fixes. We've turned our bodies into chemical experiments. Stop the PPIs. Get tested. Your kidneys are whispering. Are you listening?
Chetan Chauhan
December 5, 2025 AT 11:31uuhh so ppi's bad but what about antacids?? i mean like tums?? are they safe?? or is evrything bad now??
Phil Thornton
December 6, 2025 AT 19:27I’ve been on ibuprofen for my back for 5 years. No symptoms. No warning. Just a blood test that said ‘your kidneys are sad.’ I didn’t even know I was in danger until it was almost too late.
Pranab Daulagupu
December 8, 2025 AT 10:24AIN is a silent epidemic fueled by polypharmacy. Early detection via eGFR monitoring is the only scalable solution. We need primary care protocols-not just reactive biopsies. Prevention > intervention.
Barbara McClelland
December 8, 2025 AT 22:27If you're over 65 and on 5+ meds, please talk to your doctor about a kidney panel. Seriously. It's a 5-minute blood test. Don't wait until you're on dialysis because no one thought to check. You deserve to protect your body.
Alexander Levin
December 9, 2025 AT 05:29Big Pharma knows this. That’s why PPIs are sold like candy. They don’t care if your kidneys fail-just as long as you keep buying the next drug to fix the side effects. It’s a money machine. Wake up.
Ady Young
December 10, 2025 AT 19:57I had AIN from cipro 3 years ago. Stopped the drug, got a biopsy, didn’t take steroids. Recovered fully in 6 weeks. Now I avoid all NSAIDs and PPIs. I’m alive because I listened. If you’re on these meds and feel off-don’t ignore it. Get checked. It’s not paranoia. It’s survival.