Antidepressant Comparison Tool
Use this tool to compare antidepressants based on your specific needs and preferences.
Enter your preferences and click "Compare Options" to see the best-suited antidepressant for you.
Ever stared at a pharmacy shelf and wondered whether the blue pill labeled Fluoxetine is really the best fit for your mood‑boosting needs? You’re not alone. Millions of people with major depressive disorder (MDD) wrestle with the same question every time a doctor mentions an antidepressant. Below you’ll get a straight‑talk, side‑by‑side look at fluoxetine, its close cousins, and the non‑drug routes that often get overlooked.
Key Takeaways
- Fluoxetine’s ultra‑long half‑life (4‑6 days) means fewer withdrawal headaches but a slower start for some.
- Sertraline and escitalopram typically kick in faster, yet they may cause more sexual side effects.
- SNRIs such as venlafaxine offer stronger pain relief but can raise blood pressure.
- Therapies like CBT work without medication, making them ideal adjuncts or first‑line options for mild‑to‑moderate depression.
- Switching drugs is safest when done under doctor supervision, using taper‑and‑cross‑over strategies.
What Is Fluoxetine?
Fluoxetine, sold under the brand name Prozac, belongs to the selective serotonin reuptake inhibitor (SSRI) family. It works by blocking the serotonin transporter, allowing more serotonin to linger in the synaptic gap and improve mood. Typical adult dosing starts at 20mg once daily, with a maintenance range of 20‑80mg. Its standout attribute is a half‑life of 4‑6 days-one of the longest among SSRIs-so the drug hangs around in your system for weeks after you stop taking it. This long tail reduces the risk of abrupt discontinuation symptoms but can delay full therapeutic effect for up to 4‑6 weeks.
Key attributes of fluoxetine include:
- Class: SSRI
- Typical dose: 20‑80mg/day
- Half‑life: 4‑6 days (active metabolite desmethyl‑fluoxetine adds another 7‑9 days)
- Common side effects: insomnia, dry mouth, headache, occasional GI upset
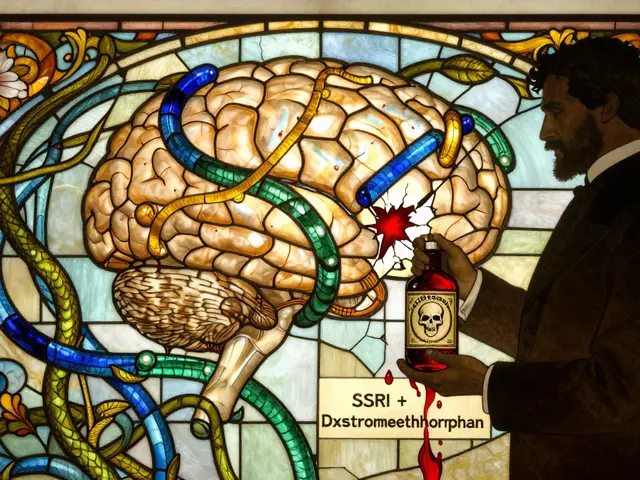
- Drug interactions: heightened risk with MAO inhibitors, certain anti‑coagulants, and triptans
Major Alternatives at a Glance
Before you pick a winner, let’s meet the main players that show up in most prescribing charts.
- Sertraline - another SSRI, known for a slightly faster onset and stronger anxiety relief.
- Citalopram - a once‑daily SSRI with a clean side‑effect profile but a dose ceiling of 40mg due to QT‑interval concerns.
- Escitalopram - the S‑enantiomer of citalopram; often hailed as the most potent SSRI per milligram.
- Paroxetine - an SSRI that doubles as a strong antihistamine, useful for patients with concurrent allergy symptoms but notorious for weight gain.
- Venlafaxine - a serotonin‑norepinephrine reuptake inhibitor (SNRI) that adds norepinephrine boost, helping with chronic pain and severe depression.
- Duloxetine - another SNRI, often chosen for its dual action on mood and neuropathic pain.
- Cognitive Behavioral Therapy (CBT) - a non‑pharmacologic, structured talk therapy proven to reduce depressive symptoms in 50‑60% of patients when delivered weekly for 12‑20 sessions.
Direct Comparison Table
| Drug / Option | Class | Typical Starting Dose | Half‑life (days) | Common Side Effects | Special Considerations |
|---|---|---|---|---|---|
| Fluoxetine | SSRI | 20mg QD | 4‑6 (plus metabolite 7‑9) | Insomnia, dry mouth, GI upset | Long wash‑out; low discontinuation syndrome |
| Sertraline | SSRI | 50mg QD | ≈1‑2 | Diarrhea, sexual dysfunction, jitteriness | Good for anxiety; may cause more sexual side effects |
| Escitalopram | SSRI | 10mg QD | ≈1‑2 | Nausea, fatigue, sexual dysfunction | Highest potency; low dosing needed |
| Venlafaxine | SNRI | 37.5mg QD | ≈5 | Increased blood pressure, sweating, nausea | Effective for pain; monitor BP |
| Duloxetine | SNRI | 30mg QD | ≈12 | Dry mouth, constipation, liver enzyme rise | Beneficial for diabetic neuropathy |
| CBT (12‑20 sessions) | Psychotherapy | N/A | N/A | Time commitment, therapist availability | No drug interactions; durable relapse prevention |
How to Choose the Right Option
Picking an antidepressant isn’t a lottery; it’s a balance of several personal factors. Use this checklist to narrow down the choices that line up with your lifestyle and health profile.
- Speed of symptom relief. If you need a quicker lift, sertraline or escitalopram’s shorter half‑life may feel faster than fluoxetine’s gradual climb.
- Side‑effect tolerance. Sexual dysfunction is a common complaint with many SSRIs. Venlafaxine often sidesteps this but can raise blood pressure, so regular monitoring is a must.
- Existing medical conditions. Patients on blood thinners or with cardiac QT concerns should avoid high‑dose citalopram and consider fluoxetine or an SNRI with cardiac safety data.
- Drug‑interaction landscape. Fluoxetine’s long half‑life can linger, complicating switches to medications metabolized by CYP2D6. If you’re on a poly‑drug regimen, a shorter‑acting SSRI like sertraline may be safer.
- Cost and insurance coverage. Generic fluoxetine is often the cheapest SSRI. SNRIs and newer SSRIs can be pricier, though many plans cover them after a prior‑auth step.
- Preference for non‑drug approaches. If you value a medication‑free strategy, CBT or regular aerobic exercise can achieve remission rates comparable to mild‑to‑moderate SSRI therapy.
Talk these points through with your prescriber-your input helps tailor the regimen.
Non‑Medication Alternatives Worth Considering
Medication isn’t the only route to lift the fog. Below are three evidence‑backed options that can stand alone or complement a pill.
- CBT - Structured, goal‑oriented talk therapy that teaches coping skills. A meta‑analysis of 115 trials found an average 50% remission rate for moderate depression.
- Exercise - 30 minutes of moderate aerobic activity most days boosts endorphins and serotonin. The British Journal of Sports Medicine reported a 25% reduction in depressive scores after 12 weeks of regular jogging.
- Omega‑3 fatty acids - EPA‑rich fish oil supplements have shown modest mood benefits, especially in patients who don’t respond fully to SSRIs.
These strategies are low‑risk and can improve overall wellbeing, making them smart additions to any treatment plan.
Switching or Combining Treatments Safely
Sometimes the first pick isn’t a perfect match. Here’s a practical roadmap for a smooth transition.
- Consult your doctor. Never stop a medication abruptly; a taper prevents withdrawal symptoms.
- Plan a cross‑taper. For fluoxetine to sertraline, reduce fluoxetine by 20mg every week while introducing sertraline at a low dose (25mg). The overlap period leverages fluoxetine’s lingering half‑life.
- Monitor side effects. Keep a daily log of mood, sleep, appetite, and any new physical sensations. Share the log at follow‑up appointments.
- Adjust dosage. Most SSRIs hit a therapeutic plateau at 4-6 weeks. If symptoms linger, your prescriber may increase the dose or add an adjunct (e.g., low‑dose bupropion for energy).
- Consider augmentation with psychotherapy. Even a brief 6‑session CBT course can boost response rates when paired with medication.
Remember, the goal isn’t just to find a drug that works-it’s to create a sustainable plan that fits your life.

Frequently Asked Questions
How long does it take for fluoxetine to start working?
Most people notice a subtle mood lift after 2‑4 weeks, but full therapeutic effect can take 4‑6 weeks because fluoxetine builds up slowly in the bloodstream.
Is fluoxetine safe to take with alcohol?
Occasional light drinking isn’t contraindicated, but heavy alcohol can worsen side effects like insomnia and increase the risk of liver strain. Discuss your drinking habits with your doctor.
Can I switch from fluoxetine to an SNRI without a wash‑out period?
Because fluoxetine lingers, a short wash‑out (about 1‑2 weeks) is usually recommended before starting an SNRI like venlafaxine. Your doctor may opt for a slower cross‑taper to avoid serotonin syndrome.
Why do some people experience weight gain on fluoxetine?
Weight changes are individual. Fluoxetine’s activating effect often leads to appetite suppression early on, but as mood improves, appetite can normalize, sometimes resulting in modest weight gain. Monitoring diet and activity helps manage this.
Is CBT effective for severe depression, or only mild cases?
CBT works across the spectrum. In severe cases, it’s most powerful when combined with medication, but several trials show CBT alone can lead to remission in up to 40% of severe patients.





Aayush Shastri
September 29, 2025 AT 19:33Fluoxetine’s long half‑life can be a blessing for patients who travel frequently across time zones, especially in a country as diverse as India where access to pharmacies may vary.
When cost is a concern, the generic version remains one of the most affordable SSRIs on the market.
However, clinicians should still screen for insomnia, as the activating effect can clash with the hot climate and altered sleep patterns.
If you have a history of cardiac issues, the lower risk of QT prolongation makes fluoxetine a safer SSRI compared to citalopram.
Always discuss any herbal supplements, such as ayurvedic preparations, with your doctor to avoid unexpected interactions.
Benton Myers
September 30, 2025 AT 17:46Fluoxetine works slower but hangs around longer, which can be handy if you forget a dose.
Pat Mills
October 1, 2025 AT 16:00In the grand tapestry of American psychiatric practice, fluoxetine has long stood as the flagship of the SSRIs, a true product of our innovative drug development pipeline. Its half‑life, stretching over five days, offers a stability that mirrors the steadfast resilience of our nation. While other agents such as sertraline sprint onto the scene like fleeting fireworks, fluoxetine marches on with deliberate purpose, much like the slow but sure march of American progress. Critics who bemoan its delayed onset fail to recognize that patience is a virtue deeply embedded in the American spirit. Moreover, the low discontinuation syndrome associated with fluoxetine reflects the nation's commitment to continuity and reliability. When it comes to side‑effects, the occasional insomnia or dry mouth are minor inconveniences compared to the tumult of economic and social upheavals we face daily. The drug’s metabolic pathway via CYP2D6 is well‑characterized, allowing clinicians across the United States to tailor dosages with confidence. Patients with a history of hypertension should note that fluoxetine's minimal impact on blood pressure makes it a superior choice over many SNRIs that threaten to raise systolic numbers. For those concerned about sexual dysfunction, fluoxetine’s comparatively milder sexual side‑effect profile can be a strategic advantage in sustaining long‑term adherence. The financial accessibility of generic fluoxetine, often priced in pennies per tablet, exemplifies the American dedication to affordable healthcare. In contrast, newer agents such as vortioxetine carry premium price tags that can strain even well‑insured individuals. From a pharmacogenomic perspective, fluoxetine’s long‑acting metabolite desmethyl‑fluoxetine serves as a safety net, preventing abrupt withdrawal that could destabilize a patient’s life. Clinicians must, however, remain vigilant about drug‑drug interactions, especially with warfarin or triptans, since the United States boasts a high prevalence of polypharmacy. The integration of fluoxetine into multidisciplinary treatment plans, pairing it with evidence‑based CBT, showcases the holistic approach championed by American mental health institutions. Thus, when weighing the options, fluoxetine stands not only as a medication but as a symbol of the United States’ enduring quest for balanced, effective, and accessible mental health care.
jennifer jackson
October 2, 2025 AT 14:13Fluoxetine can be a solid first step for many; it’s reliable and often affordable.
Alec McCoy
October 3, 2025 AT 12:26When you’re weighing fluoxetine against alternatives, start by listing what matters most to you-speed of relief, side‑effect tolerance, or cost.
For patients who can wait a few weeks for mood improvement, fluoxetine’s long half‑life offers the advantage of fewer withdrawal headaches if a dose is missed.
If rapid anxiolytic effect is a priority, sertraline or escitalopram may feel quicker, though they sometimes bring more sexual side‑effects.
Remember that SNRIs such as venlafaxine can address both depression and chronic pain, but they require regular blood pressure checks.
Non‑pharmacologic options like CBT or regular aerobic exercise can be combined with any medication to boost response rates.
Talk openly with your prescriber about any herbal supplements or over‑the‑counter meds you’re taking; even something as common as St. John’s wort can shift serotonin levels.
Ultimately, the best choice is the one you can stick with consistently while feeling empowered in your treatment journey.
Aaron Perez
October 4, 2025 AT 10:40Consider, dear reader, the paradox of prescribing fluoxetine: a molecule that whispers slow serenity, yet demands a patient’s unwavering commitment; this duality mirrors life’s own cadence, a rhythm of anticipation and delayed gratification.
One must weigh the pharmacokinetic elegance-its 4‑6‑day half‑life, the lingering desmethyl metabolite-against the psychological yearning for immediate uplift; this equilibrium is not merely clinical, it is existential.
Critically, the practitioner’s role extends beyond the pill, encompassing a stewardship of hope, a guard against the chaos of polypharmacy, and a vigilant eye on interactions with anticoagulants, triptans, and even certain antihistamines.
In the grand tapestry of treatment, fluoxetine offers a stable thread, yet it is the therapist’s needle, the patient’s will, and the environment that weave the ultimate outcome.
Thus, the decision to initiate fluoxetine should be ensconced within a holistic schema, integrating lifestyle, comorbidities, and the inexorable march toward wellness.
William Mack
October 5, 2025 AT 08:53The longer half‑life of fluoxetine can be beneficial for patients with irregular dosing schedules.
Evan Riley
October 6, 2025 AT 07:06Many pharma giants push newer, expensive antidepressants claiming faster relief, yet they conveniently downplay fluoxetine’s solid track record, hoping we’ll chase profit over proven stability.
The marketing machine often hides the fact that fluoxetine’s side‑effect profile is comparatively mild, while newer agents bring hidden cardiovascular risks.
Don’t be fooled by glossy advertisements; a seasoned clinician knows that the old‑school SSRIs still hold the gold standard for many.
Nicole Povelikin
October 7, 2025 AT 05:20i think people overrate fluoxetene and forget that some folks feel better on older tricyclics even tho they have more side effects.
Michelle Weaver
October 8, 2025 AT 03:33Fluoxetine remains a cost‑effective option for many patients 🌟 its long half‑life reduces the need for frequent dose adjustments 🌟 clinicians should monitor for insomnia and dry mouth while considering drug interactions 🌟 combining the medication with CBT can enhance remission rates 🌟
John Keough
October 9, 2025 AT 01:46When evaluating fluoxetine versus sertraline, it helps to consider both pharmacokinetics and patient lifestyle; fluoxetine’s extended half‑life reduces daily pill burden, while sertraline may provide quicker symptom relief.
Discussing these nuances with a mental‑health provider enables a tailored plan that respects individual preferences and clinical evidence.
Graham Smith
October 10, 2025 AT 00:00The article contains several typographical errors, such as “fluoxetine” instead of “fluoxetine” and inconsistent use of “SSRI” capitalization; correcting these improves readability and professional credibility.
Jeremiah Morgan
October 10, 2025 AT 22:13It is commendable that you are seeking a comprehensive understanding of antidepressant options; such diligence often correlates with improved adherence and therapeutic outcomes.
Should you elect fluoxetine, be assured that its extensive safety data and affordability render it a prudent first‑line choice for many individuals.