TL;DR
- Alcohol can irritate the bladder and worsen urgency.
- Limit intake to 1‑2 drinks per day and avoid binge drinking.
- Stay hydrated with water, not just alcohol, to keep urine concentrated.
- Talk to your doctor before mixing alcohol with bladder meds.
- Track drinks and bathroom trips in a bladder diary for better control.
Overactive Bladder is a chronic condition marked by a sudden, uncontrollable urge to urinate, often accompanied by frequency and nocturia. It affects roughly 16% of adults worldwide, according to recent urology surveys, and its impact on daily life can be significant.
When you add Alcohol to the mix, the picture changes. Alcohol is a known diuretic that increases urine production by inhibiting the antidiuretic hormone (ADH). More urine means a fuller bladder faster, which can trigger the symptoms of overactive bladder.
Why Alcohol Triggers Urinary Urgency
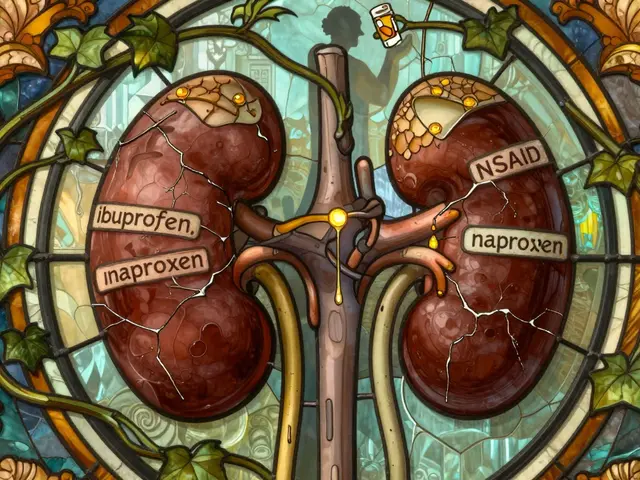
The chain reaction starts with the detrusor muscle, the smooth muscle lining the bladder wall. In a healthy bladder, the detrusor stays relaxed while filling and contracts only when it’s time to empty. Alcohol interferes with this balance in three ways:
- Increased urine volume: By suppressing ADH, alcohol lets the kidneys release more water.
- Reduced bladder capacity: Alcohol irritates the bladder lining, making it less tolerant of stretch.
- Heightened nerve sensitivity: Ethanol can amplify the signals sent from bladder stretch receptors to the brain.
These mechanisms explain why a single beer or glass of wine can turn a calm evening into a sprint to the bathroom.
Comparing Alcohol and Other Common Triggers
| Attribute | Alcohol | Caffeine |
|---|---|---|
| Primary active compound | Ethanol | Caffeine |
| Diuretic strength (relative) | High | Moderate |
| Typical impact on urgency | Increases frequency and urgency | May increase urgency, especially in sensitive individuals |
| Recommended limit for OAB sufferers | ≤ 1‑2 drinks/day, avoid binge | ≤ 200mg caffeine (≈2 cups coffee) per day |
| Interaction with anticholinergic meds | Can amplify side‑effects (dry mouth, constipation) | Generally neutral, but high doses may worsen symptoms |
How Alcohol Interacts with Common OAB Treatments
Many patients rely on anticholinergic medication such as oxybutynin or tolterodine to calm an overactive detrusor. These drugs work by blocking the acetylcholine receptors that tell the muscle to contract.
When you drink alcohol while on anticholinergics, two things can happen:
- Exacerbated side‑effects: Both alcohol and anticholinergics cause dry mouth and constipation. Together they can become uncomfortable.
- Reduced drug efficacy: Alcohol can alter liver enzymes, potentially changing how quickly the medication is broken down.
Clinical guidelines from urology societies advise patients to discuss any drinking habits with their physician before starting medication.
Practical Strategies to Keep Drinking Safe
If you love a weekend glass of red, you don’t have to quit outright. The key is moderation and timing:
- Set a clear limit: Stick to no more than one standard drink (12oz beer, 5oz wine, 1.5oz spirits) per day for women, two for men. This aligns with CDC recommendations and helps keep urine production manageable.
- Hydrate before and after: Drink a glass of water for every alcoholic beverage. This dilutes the urine and reduces irritation.
- Avoid binge patterns: Consuming three or more drinks in an hour spikes diuresis and often overwhelms the bladder’s capacity.
- Choose low‑alcohol options: Light beers (≈3% ABV) or wines with lower alcohol by volume produce less diuretic effect.
- Schedule bathroom breaks: Empty the bladder every 2‑3hours during drinking sessions to prevent over‑filling.

Integrating Lifestyle Tools for Better Control
Beyond drink limits, a few habit tweaks can make a big difference:
- Pelvic floor muscle training: Strengthening these muscles improves bladder control. Simple Kegel exercises, done three times daily, have been shown in randomized trials to reduce urgency episodes by up to 30%.
- Bladder diary keeping: Recording fluid intake, alcohol consumption, and bathroom trips for a week reveals patterns you can tweak.
- Fluid intake guidelines: Aim for 1.5‑2L of water daily, spaced throughout the day. Avoid large volumes within two hours of bedtime to lessen nocturia.
- Urodynamic testing for unclear cases: If symptoms persist despite lifestyle changes, this office‑based test measures bladder pressure and capacity, helping doctors tailor therapy.
When to Seek Professional Help
Not all urgency is caused by alcohol. If you notice any of these red flags, schedule a urology appointment:
- Blood in urine or a sudden change in odor.
- Painful urination or a burning sensation.
- Frequent nighttime trips (more than twice per night).
- Inability to hold urine even after limiting alcohol.
Early evaluation can rule out infections, stones, or neurological issues that require specific treatment.
Bottom Line: Balance Overrestriction with Informed Choices
Alcohol isn’t a death sentence for people with overactive bladder, but it does demand mindful consumption. By staying within moderate limits, hydrating wisely, and pairing drinking with bladder‑friendly habits, you can keep urgency under control without giving up social enjoyment.
Frequently Asked Questions
Can a single drink worsen overactive bladder symptoms?
Yes. Even one standard drink can trigger a noticeable increase in urinary frequency for many sufferers because ethanol acts as a potent diuretic.
Is it safe to drink wine while taking anticholinergic medication?
Moderate wine consumption (one glass) is generally safe, but you should discuss your drinking habits with your doctor. Alcohol can heighten dry‑mouth and constipation side‑effects.
How many drinks per week are considered low‑risk for OAB?
Limiting intake to 7 drinks for women and 14 drinks for men per week (roughly 1‑2 drinks per day) stays within most health guidelines and minimizes bladder irritation.
Does non‑alcoholic beer affect the bladder the same way?
Most non‑alcoholic beers contain very low ethanol levels, so their diuretic impact is minimal. However, carbonation can still irritate a sensitive bladder for some people.
What lifestyle changes help reduce urgency besides limiting alcohol?
Practice pelvic floor (Kegel) exercises, keep a bladder diary, stay well‑hydrated with water, avoid bladder irritants like caffeine and artificial sweeteners, and maintain a regular voiding schedule.
Can binge drinking cause long‑term bladder damage?
Repeated binge episodes can lead to chronic inflammation of the bladder lining, increasing the risk of urinary tract infections and potentially worsening overactive bladder over time.




A Walton Smith
September 25, 2025 AT 21:56Alcohol just makes OAB worse.
Iván Cañas
October 5, 2025 AT 04:15Totally agree that staying hydrated with water between drinks can really help keep the bladder from getting too irritated. Drinking a glass of water after each alcoholic beverage is a simple trick that many people forget, and it can make a big difference in how often you need to run to the bathroom.
Lily Tung
October 14, 2025 AT 10:34It is essential to understand the physiological mechanisms behind alcohol induced urgency in overactive bladder. Ethanol suppresses antidiuretic hormone resulting in increased urine output. This diuretic effect fills the bladder more quickly than usual. The detrusor muscle receives stronger stretch signals as a result. Nerve pathways become sensitized to these signals. Consequently the brain interprets bladder fullness earlier. Even a single standard drink can trigger this cascade. Repeated exposure can condition the bladder to react more aggressively. Patients often report a noticeable increase in nocturia after a night of drinking. The increased frequency can interfere with sleep quality and daily productivity. Moreover alcohol can irritate the urothelium reducing its capacity to stretch. This irritation may persist beyond the immediate metabolic effects of alcohol. When combined with anticholinergic medication the side effect profile can worsen. Dry mouth constipation and reduced drug efficacy are common concerns. Therefore moderation is not merely a recommendation but a necessity for optimal management. Incorporating these insights into a personalized plan can empower individuals to maintain social enjoyment while protecting bladder health.
Xander Laframboise
October 23, 2025 AT 16:53While hydrating sounds reasonable it doesn’t address the core issue that alcohol itself is a potent bladder irritant. No amount of water can fully counteract the diuretic spike caused by ethanol, so the focus should be on limiting intake rather than just adding water.
Jason Petersen
November 1, 2025 AT 22:12yeah limit is key but most people ignore it
Melissa Gerard
November 11, 2025 AT 04:31Honestly I think the whole “moderate drinking” myth is just marketing fluff :)
Rebecca Fuentes
November 20, 2025 AT 10:50From a clinical perspective the recommendation to cap alcohol consumption at one to two drinks per day aligns with epidemiological data indicating a threshold beyond which urinary symptoms exacerbate significantly. Moreover, individualized counseling that considers patient-specific factors such as concurrent medication regimens can enhance adherence to these guidelines. Integrating bladder diaries into routine follow‑up appointments provides objective metrics for both patients and clinicians to assess the impact of alcohol on symptom frequency. This systematic approach facilitates evidence‑based adjustments to lifestyle and pharmacotherapy, ultimately improving quality of life for individuals coping with overactive bladder.
Jacqueline D Greenberg
November 29, 2025 AT 17:09Thanks for the detailed breakdown! I’ve started keeping a diary and already see a drop in midnight trips when I stick to the limits.
Jim MacMillan
December 8, 2025 AT 23:28Honestly the science is crystal clear 📊 Alcohol spikes diuresis and that’s a recipe for urgency 🍺🚽 So if you want to keep your bladder happy just keep the drinks low and stay hydrated 💧👍
Dorothy Anne
December 18, 2025 AT 05:47Exactly! Small changes add up big time. Keep crushing those limits and watch your symptoms fade!
Sharon Bruce
December 27, 2025 AT 12:05Our country’s health guidelines already warn against excess booze – follow them.
True Bryant
January 5, 2026 AT 18:24In the grand tapestry of modern medicine, the reckless indulgence in ethanol stands as a flagrant affront to the sanctity of urological equilibrium. The nefarious interplay between acetylcholine antagonists and alcohol metabolites precipitates a cascade of iatrogenic complications that the layperson scarcely comprehends. One must recognize that the reckless consumption of spirits not only undermines therapeutic efficacy but also egregiously violates the Hippocratic Oath of “do no harm.” Therefore, it is incumbent upon the enlightened patient to eschew intemperance and embrace disciplined moderation.
Danielle Greco
January 15, 2026 AT 00:43Great point! Just a tiny edit – “eschew” is perfect, but maybe swap “intemperance” with “excess drinking” for clarity 😊
Linda van der Weide
January 24, 2026 AT 07:02When we contemplate the relationship between spirituous libations and bladder dynamics we are, in essence, confronting the paradox of pleasure versus physiological cost. The fleeting euphoria derived from a glass of wine is shadowed by the inevitable urgency that follows, a reminder that our bodies negotiate every indulgence with a silent ledger of consequences. Yet, this dance is not merely binary; it invites a nuanced discourse on personal thresholds, societal norms, and the ever‑present whisper of medical guidance. By embracing a reflective stance, individuals can navigate the delicate balance between enjoyment and health without succumbing to either extremity.
Philippa Berry Smith
February 2, 2026 AT 13:21Sure, but you’ll never hear the pharma companies admit they push anti‑alcohol meds to keep us dependent.
Joel Ouedraogo
February 11, 2026 AT 19:40Ask yourself: if a single sip can double your bathroom trips, why gamble with comfort?
Beth Lyon
February 21, 2026 AT 01:59i think its suuper personal decision lol