Progesterone Level Age Tracker
Estimated Progesterone Level
When we talk about Progesterone is a steroid hormone primarily produced by the ovaries that readies the uterus for pregnancy and helps balance the menstrual cycle, the conversation often stops at fertility. Yet progesterone levels don’t stay constant throughout life. As we get older, the hormone’s production, timing, and impact shift in ways that touch everything from bone strength to mood. This article uncovers what those changes look like, why they matter, and practical steps you can take to stay in sync with your body.
Key Takeaways
- Progesterone peaks after ovulation and drops sharply if pregnancy doesn’t occur; this rhythm blunts after age 35.
- Typical serum ranges shrink with age, especially once menopause begins.
- Low progesterone can affect fertility, bone density, cardiovascular health, and emotional well‑being.
- Lifestyle tweaks-adequate sleep, balanced diet, stress control-help support natural production.
- Medical options such as hormone replacement therapy (HRT) are available, but timing and dosage should be personalized.
How Progesterone Works in the Body
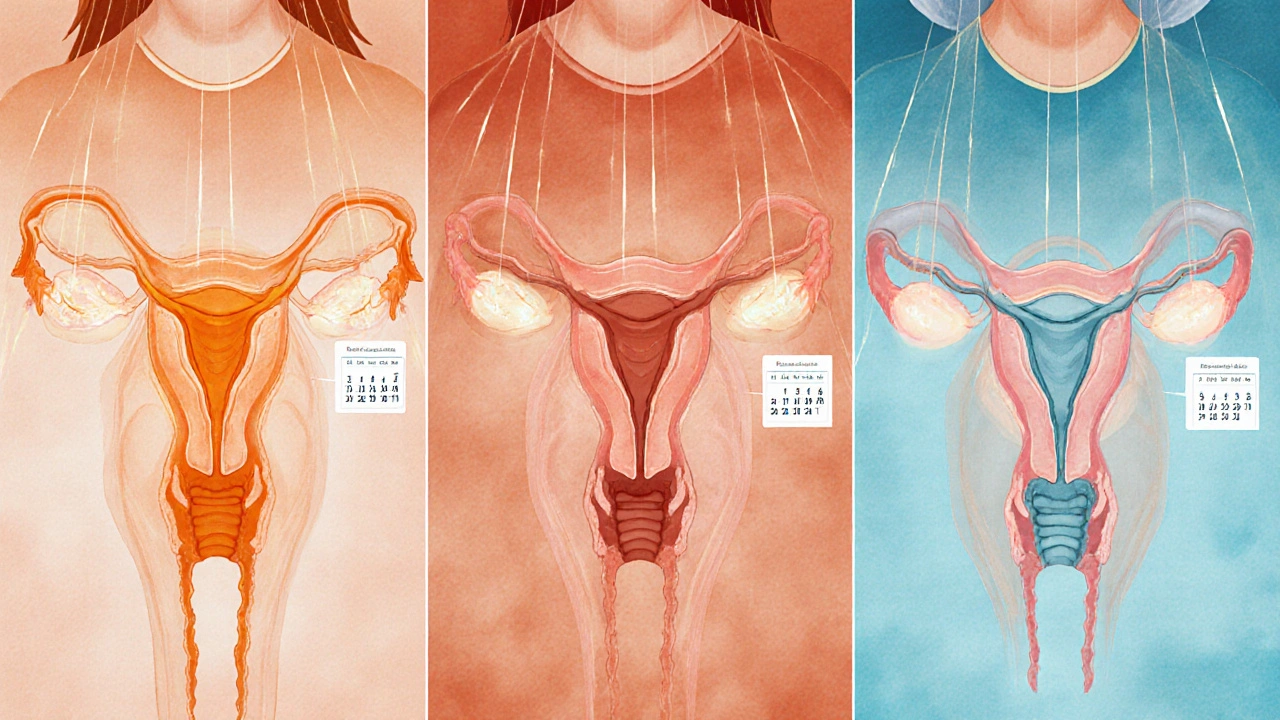
After the follicle releases an egg, the Luteal Phase is the short window where the ruptured follicle transforms into the corpus luteum, pumping out progesterone to thicken the uterine lining. If fertilization fails, the hormone drops, triggering menstruation.
While the ovaries are the main source, the Adrenal Glands contribute a modest amount, especially during stress. The hormone works hand‑in‑hand with Estrogen, another ovarian steroid that drives the first half of the cycle. Together they keep the reproductive system humming and also influence mood, sleep, and metabolic rate.

Age‑Related Changes in Progesterone Levels
Women in their 20s typically see a luteal‑phase serum range of 5-20ng/mL. By the mid‑30s, the upper end often trims down to about 12ng/mL, and the curve becomes flatter. After the Menopause transition (average age 51 in the UK), ovarian output plummets, leaving only the adrenal trickle-usually below 5ng/mL.
| Age Group | Typical Range | Main Source | Key Function |
|---|---|---|---|
| 20‑29 | 5‑20 | Ovaries (corpus luteum) | Prepare uterus for implantation |
| 30‑39 | 4‑15 | Ovaries (corpus luteum) | Maintain luteal phase stability |
| 40‑49 | 3‑12 | Ovaries + adrenal | Support bone turnover, mood |
| 50‑59 (post‑menopause) | 1‑5 | Adrenal glands | Minor metabolic roles |
| 60+ | <1 | Adrenal glands | Negligible reproductive impact |
These numbers illustrate the steady decline. The shifts matter because progesterone isn’t just a “pregnancy hormone.” Its drop triggers downstream changes that can affect overall health.
Health Implications of Declining Progesterone
Fertility: Lower luteal‑phase peaks make it harder for the uterine lining to stay receptive, reducing implantation odds. Many women in their late 30s notice shorter luteal phases and more frequent spotting.
Bone Density: Progesterone works with estrogen to stimulate osteoblast activity-the cells that build bone. As levels dip, especially after menopause, the protective effect weakens, contributing to osteoporosis risk. Studies from the British Osteoporosis Society show a 15‑20% higher fracture rate in women with persistently low progesterone post‑menopause.
Cardiovascular Health: Emerging data link low progesterone to increased arterial stiffness and higher LDL cholesterol. While estrogen has been the star of heart‑health research, progesterone’s role in modulating blood vessel tone is gaining attention.
Mood and Sleep: The hormone binds to GABA receptors in the brain, promoting calm. Decline can lead to irritability, anxiety, and even night‑time awakenings. Women often report “menopause brain fog” that mirrors low‑progesterone symptoms.
Managing Progesterone Decline Naturally
Before reaching for medication, consider these lifestyle levers:
- Nutrition: Foods rich in zinc (pumpkin seeds, oysters) and vitamin B6 (bananas, chickpeas) support progesterone synthesis.
- Healthy Fats: Cholesterol is the building block for all steroid hormones. Avocado, olive oil, and fatty fish keep the raw material pool adequate.
- Stress Reduction: Chronic cortisol from the adrenal glands can divert precursors away from progesterone. Mindfulness, yoga, and regular moderate exercise help keep cortisol in check.
- Sleep Hygiene: Deep sleep spikes growth hormone, which indirectly supports overall hormone balance. Aim for 7‑9 hours, limit screens before bed.
- Weight Management: Excess adipose tissue can convert progesterone into cortisol, further lowering circulating levels.
If lifestyle tweaks aren’t enough, consult a healthcare professional about targeted options.

Medical Options: Hormone Replacement Therapy
When natural methods fall short, Hormone Replacement Therapy (HRT) can restore a more youthful hormonal profile. Traditional HRT combos often pair estrogen with a synthetic progestogen to protect the uterus from hyperplasia. However, newer bioidentical progesterone preparations (micronized oral capsules, transdermal gels, or vaginal suppositories) aim to mimic the body’s own hormone more closely.
Key considerations:
- Timing: Starting HRT within 10 years of menopause onset (the “window of opportunity”) appears to yield the best cardiovascular and bone outcomes.
- Dosage: The goal is to achieve luteal‑phase‑like serum levels (around 5‑10ng/mL). Doctors usually begin with low doses and titrate based on symptoms and blood tests.
- Formulation Choice: Transdermal routes bypass first‑pass liver metabolism, reducing clot risk compared with oral estrogen‑only regimens.
Always discuss potential risks-breast tenderness, mood changes, and rare clotting events-with your clinician. Individualized care is essential.
When to Seek Professional Guidance
Persistent symptoms such as irregular periods, difficulty conceiving, frequent bone fractures, or sudden mood swings warrant a hormone evaluation. A simple serum test can map your current Progesterone level, estrogen, and follicle‑stimulating hormone (FSH) to pinpoint where you stand.
Ask your GP or a specialist about:
- Baseline hormone panel and follow‑up schedule.
- Bone density scan (DEXA) if you’re over 50 or have a family history of osteoporosis.
- Cardiovascular risk assessment, especially if you have a smoking history or high cholesterol.
Early detection lets you address declines before they evolve into bigger health concerns.
Frequently Asked Questions
How do I know if my progesterone is low?
Common clues include shorter luteal phases, irregular spotting, difficulty getting pregnant, sudden anxiety or sleep disruption, and early signs of bone loss. A blood test taken about a week after ovulation provides the most accurate reading.
Can lifestyle changes really raise progesterone?
Yes. Adequate zinc and vitamin B6, regular moderate exercise, stress‑management techniques, and healthy fats have all been shown in clinical nutrition studies to support the body’s steroid‑hormone pathways, leading to modest increases in luteal‑phase progesterone.
Is bioidentical progesterone safer than synthetic progestins?
Current research suggests bioidentical forms align more closely with natural hormone receptors, resulting in fewer side‑effects such as breast tenderness or mood swings. However, safety still depends on dose and personal health history, so medical supervision is essential.
Will low progesterone affect my heart health?
Lower progesterone is linked to higher LDL cholesterol and reduced arterial flexibility, modestly increasing cardiovascular risk. Pairing hormone support with a heart‑healthy diet and regular cardio exercise can offset these effects.
Should I start HRT as soon as I hit menopause?
Timing matters. Starting HRT within the first decade after menopause offers the best balance of bone protection and heart health, according to the UK National Institute for Health and Care Excellence. Discuss personal risks-such as clotting history-before deciding.





Becky Jarboe
October 5, 2025 AT 17:16Progesterone’s trajectory across the lifespan is a classic example of endocrine dynamics, where the luteal‑phase peak gradually attenuates due to ovarian senescence and adrenal compensation. The shift from a robust 5‑20 ng/mL window to sub‑5 ng/mL post‑menopause has downstream effects on bone remodeling and neuro‑psychological health. Understanding these patterns can help us tailor lifestyle interventions before the hormonal decline becomes clinically evident.
Carl Boel
October 15, 2025 AT 15:05The decline of progesterone is just another symptom of our society’s hormonal neglect.
Shuvam Roy
October 25, 2025 AT 12:55While it is true that hormonal changes can reflect broader health trends, it is important to approach the topic with scientific rigor. Research consistently shows that progesterone modulation impacts bone density, cardiovascular risk, and mood regulation. Therefore, a nuanced view that integrates endocrinology with public health policy is essential. Moreover, evidence‑based lifestyle modifications, such as adequate zinc intake and stress management, can mitigate some of the adverse effects associated with declining progesterone levels.
Jane Grimm
November 4, 2025 AT 09:44One must commend the article’s thoroughness, yet the prose occasionally descends into vacuous platitudes rather than precise scientific exposition. The misuse of “minor metabolic roles” without quantitative backing borders on speculative rhetoric. Moreover, the table’s formatting betrays a lack of editorial discipline, which undermines the credibility of the purported data. In sum, while the intent is laudable, the execution demands stricter adherence to scholarly standards.
Nora Russell
November 14, 2025 AT 07:33The previous comment highlights valid concerns regarding editorial precision, yet it neglects to address the substantive content concerning progesterone’s systemic impact. A more constructive critique would acknowledge the article’s accurate synthesis of endocrine pathways while proposing enhancements, such as integrating recent meta‑analyses on HRT cardiovascular outcomes. Additionally, the argument would benefit from a clearer delineation between adrenal and ovarian contributions post‑menopause.
Craig Stephenson
November 24, 2025 AT 05:22Great rundown! For anyone looking to boost natural progesterone, I’ve found that adding pumpkin seeds and chickpeas to meals really helps. Also, try to get consistent 7‑9 hours of sleep; deep sleep spikes growth hormone which indirectly supports hormone balance. Small changes add up, so keep at it!
Tyler Dean
December 4, 2025 AT 03:11Honestly, all these “natural hacks” are just distractions from the real control mechanisms. The pharma industry manipulates data to keep us buying synthetic hormones.
Anuj Ariyo
December 14, 2025 AT 01:00Interesting read; the data tables are quite informative, however, the script’s conditional logic seems off-age >= 20 && age = 40 && age = 50? That could cause inaccurate estimates.
Tom Lane
December 23, 2025 AT 22:49You’re right about the script; fixing the conditional checks will improve the calculator’s reliability. Also, consider adding a tooltip that explains why progesterone ranges shrink with age-this will help users understand the physiology behind the numbers.
Andrea Jacobsen
January 2, 2026 AT 20:38I appreciate how the article ties hormone levels to everyday health topics like mood and bone strength. It makes the science feel relevant to our daily lives.
Andrew Irwin
January 12, 2026 AT 18:27Exactly, connecting the dots helps demystify what can seem like abstract endocrine concepts. It also encourages proactive health monitoring.
Jen R
January 22, 2026 AT 16:16First off, let’s get one thing straight: progesterone isn’t just a “pregnancy hormone” that some article decides to treat like a side note. It’s a central player in a cascade of endocrine events that affect everything from bone remodeling to cardiovascular health. When you read that the typical serum range drops from 5‑20 ng/mL in a woman’s twenties down to under 1 ng/mL after sixty, you’re looking at a profound shift in the body’s internal chemistry. That shift isn’t minor; it’s a signal that the hypothalamic‑pituitary‑ovarian axis is winding down, and the adrenal contribution, while present, is simply a backup that can’t fully compensate.
Now, let’s talk about bone health, because ignoring that fact is a disservice to anyone over forty. Progesterone works synergistically with estrogen to stimulate osteoblast activity. Lower progesterone means reduced bone formation, which, combined with the inevitable estrogen decline, spells trouble for bone density. The UK Osteoporosis Society’s data showing a 15‑20 % increase in fracture risk for post‑menopausal women with low progesterone isn’t a fluke-it’s a pattern that shows up across multiple cohorts.
Cardiovascular implications are often under‑emphasized, but emerging studies link low progesterone to increased LDL cholesterol and arterial stiffness. While estrogen has long held the spotlight, progesterone’s role in modulating vascular tone can’t be ignored. If you’re already battling high cholesterol, a dip in progesterone could tip the scales further toward atherosclerotic risk.
Mood and sleep disturbances are another piece of the puzzle. Progesterone’s metabolites, especially allopregnanolone, act on GABA‑A receptors, promoting a calming effect. A decline can manifest as irritability, anxiety, or fragmented sleep-symptoms many attribute to “menopause brain fog” but are actually rooted in neuro‑steroid deficiency.
So, what can you do about it? First, get a proper serum progesterone test timed about a week after ovulation if you’re still cycling. That gives you a realistic picture of your luteal phase. Second, address lifestyle: incorporate zinc‑rich foods (pumpkin seeds, oysters), maintain adequate healthy fats (avocado, olive oil), and prioritize stress reduction through mindfulness or gentle exercise. Third, if natural strategies fall short, discuss bioidentical progesterone options with a knowledgeable clinician-prefer transdermal or micronized oral formulations to mimic physiological patterns as closely as possible.
Finally, remember that timing matters. Starting hormone therapy within ten years of menopause has been shown to offer the best protection for bone and heart health, according to NICE guidelines. Delaying too long reduces the potential benefits and may increase risks.
In short, progesterone decline is not just a side effect of aging; it’s a pivotal factor influencing multiple health domains. Ignoring it means missing out on a key lever for maintaining overall wellness well into later life.