Levodopa Protein Timing Calculator
Your Details
Meal Planning
Results & Recommendations
Daily Protein Distribution
Based on your symptoms, we recommend:
Personalized Recommendations
Your personalized plan shows you should aim for low-protein meals during the day and higher protein in the evening to optimize medication effectiveness while maintaining nutrition.
Enter your details and meal protein distribution to see your personalized plan.
If you take Levodopaa medication used to treat Parkinson's disease that helps replenish dopamine in the brain, your protein intake might be working against you. A simple lunch of chicken and rice could reduce your medication's effectiveness by up to 40%. This isn't just a myth-it's a well-documented physiological battle happening inside your body every time you eat.
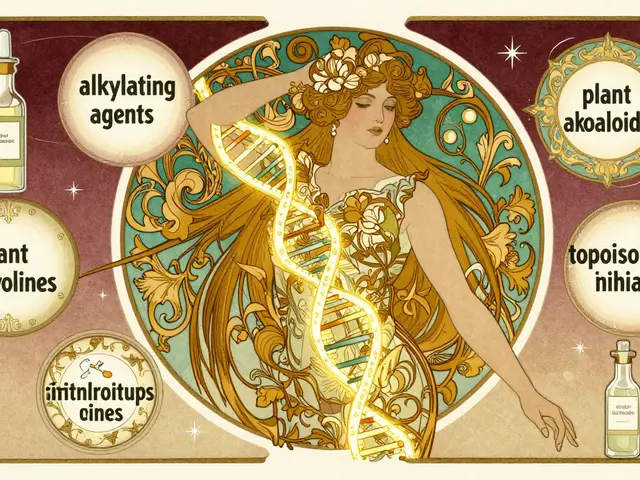
Why Protein Sabotages Your Medication
Levodopa relies on a special transport system called the LAT1 transportera carrier protein that moves large neutral amino acids across the blood-brain barrier to reach your brain. Dietary proteins break down into large neutral amino acidsincluding leucine, isoleucine, valine, phenylalanine, tyrosine, tryptophan, and methionine (LNAAs), which compete with levodopa for this same transport route. When you eat protein, these amino acids flood your bloodstream, blocking levodopa from getting where it needs to go. Studies show this competition typically starts 8-13 years after Parkinson's diagnosis or 8 years after starting levodopa therapy, affecting 40-50% of long-term users.
Imagine a busy highway where both your medication and dietary amino acids need to pass through a single toll booth. When too many amino acids arrive (like after a high-protein meal), levodopa gets stuck in traffic. This causes "off" periods-sudden loss of mobility where tremors return, stiffness worsens, and movement becomes difficult. Research from the Parkinson's Foundationa leading organization supporting Parkinson's research and patient care confirms that high-protein meals increase motor fluctuations by 32-79%, depending on the measurement scale used.
How Protein Restriction Strategies Work
Doctors now recommend three main dietary approaches to manage this conflict:
| Strategy | Protein Intake | Effectiveness | Adherence Rate |
|---|---|---|---|
| Protein Redistribution Diet (PRD) | 80-85% of daily protein in evening meal; <7g during daytime | 60.7-100% responsiveness in reducing "off" time | 68% discontinuation within 12 months |
| Low Protein Diet (LPD) | 0.6-0.8g per kg body weight daily (40-50g for 60-70kg person) | Less effective than PRD | High dropout due to nutritional issues |
| PRD with Low-Protein Products | Same as PRD, plus specialized low-protein foods | 22% higher plasma levodopa levels | Only 22% report improved satisfaction |
The most successful approach is Protein Redistribution Diet (PRD), where you eat nearly all your protein in the evening while keeping daytime meals low in protein. This strategy reduces "off" time by about 107 minutes daily and increases "on" time by 30 minutes, according to Barichella et al.'s research. It works because levodopa absorption isn't hindered when you take it on an empty stomach during low-protein daytime hours. The evening protein load doesn't interfere with nighttime doses, allowing better sleep and morning mobility.
But here's the catch: most people struggle to stick with these diets long-term. A 2023 review found 68% of patients abandon strict PRD within a year due to social pressures, food monotony, or unintended weight loss. One Reddit user (u/ParkinsonsWarrior, June 2023) shared: "After 3 months of PRD, I gained 2.5 hours of reliable mobility daily-but I had to quit when my family refused to cook two separate meals."
Real-Life Challenges and Solutions
Managing protein intake isn't just about science-it's about daily life. Parkinson's UK reports 63% of patients try protein restriction initially, but only 28% maintain it. Common pain points include:
- Social isolation: 58% of users report difficulty eating out or attending gatherings due to dietary restrictions
- Unintended weight loss: 31% lose over 5% body weight within 6 months on strict low-protein diets
- Nutritional gaps: 22% develop vitamin B12 or iron deficiencies from prolonged protein restriction
Successful strategies include:
- Taking levodopa 45 minutes before breakfast (72% success rate)
- Using "protein holidays"-one high-protein meal in the evening with careful timing
- Tracking protein with apps like MyFitnessPal (used by 47% of adherent patients)
- Substituting regular foods with low-protein alternatives (e.g., special pasta, bread, or milk substitutes)
Dr. Carley Rusch, a dietitian specializing in Parkinson's at UF Health, emphasizes: "There's no one-size-fits-all solution. A 70-year-old grandmother needs different advice than a 45-year-old athlete. We customize based on your lifestyle, weight, and symptom patterns."

What to Do Right Now
You don't need to overhaul your entire diet overnight. Start with these evidence-based steps:
- Time your doses: Take levodopa 30-60 minutes before meals or 2 hours after eating. This avoids the peak amino acid competition window.
- Track your protein: Use a food diary for one week. Note when you feel "off" periods and what you ate. You might discover patterns like "I struggle after lunch with grilled chicken" or "My morning dose works better with toast alone."
- Work with a dietitian: 78% of patients who receive professional guidance achieve better symptom control than self-managers. Ask your neurologist for a referral to a registered dietitian experienced in Parkinson's care.
- Test small changes: Try a "low-protein breakfast" for two weeks-swap eggs for oatmeal, skip bacon, and use low-protein milk alternatives. Monitor your mobility changes.
Remember: Protein restriction isn't always necessary. Only 40-50% of Parkinson's patients experience clinically significant interactions. If you're not noticing "off" periods after meals, you may not need major changes. Always consult your doctor before altering your diet or medication routine.
Frequently Asked Questions
How much protein triggers levodopa interference?
Research shows consuming more than 10 grams of protein in a single meal can significantly impact levodopa absorption. For most patients, keeping daytime protein below 7 grams per meal helps maintain medication effectiveness. However, individual tolerance varies-some people notice effects with as little as 5 grams, while others handle up to 15 grams without issues. Tracking your symptoms alongside meals is the best way to find your personal threshold.
Can I still eat meat with Parkinson's?
Yes! Meat isn't off-limits-it's about timing. Keep meat consumption for your evening meal when it won't interfere with daytime levodopa doses. For example, have a lean chicken dinner 2 hours after your last medication dose. During daytime meals, choose low-protein options like vegetables, fruits, rice, or pasta. Specialized low-protein meat substitutes are also available for those who miss traditional meat textures.
What happens if I ignore protein interactions?
Ignoring protein-levodopa interactions often leads to worsening "off" periods, unpredictable symptom control, and increased risk of dyskinesias (involuntary movements). Studies show patients who don't adjust their diet experience 32-79% more motor fluctuations, making daily tasks like walking or dressing increasingly difficult. In severe cases, this can accelerate disease progression due to inadequate dopamine replacement. However, if you don't notice symptoms after meals, you may not need changes-always monitor your body's response.
How long does it take to see improvements?
Most patients notice symptom improvements within 2-4 weeks of starting a protein management plan. For example, a 2022 study found 78% of participants had better "on" time after 3 weeks of PRD. However, full adaptation often takes 3-6 months as your body adjusts to new eating patterns. Consistency is key-tracking daily symptoms alongside meals helps identify what works best for you. If you don't see changes after 6 weeks, consult your healthcare team to adjust your approach.
Are there risks to reducing protein?
Yes, but risks are manageable with professional guidance. Strict protein restriction can lead to muscle loss, weight loss, or deficiencies in vitamin B12, iron, and zinc. To prevent this: work with a dietitian to ensure you're getting enough calories and nutrients from alternative sources; monitor your weight monthly; and consider blood tests for key vitamins and minerals every 6 months. For underweight patients (BMI under 20), protein restriction is generally not recommended-focus instead on timing medication around meals rather than reducing total protein.





Nancy Maneely
February 6, 2026 AT 12:44Levodopa and protein is a totall nightmare. I had a chicken lunch and was paralized for hours. The food industry is in cahoots with Big Pharma. But US knows better. #Drama
Phoebe Norman
February 7, 2026 AT 21:38I feel so tired all the time my body can't handle this the LAT1 transporter is overwhelmed high protein meals block levodopa I need help but no one listens
Albert Lua
February 8, 2026 AT 00:45In Japan they have a great system for protein timing. They eat most protein in the evening and have low-protein lunches. It's working well for them. I've tried it and it's helped my mobility. Everyone should look into cultural approaches! In fact, the Japanese healthcare system has been studying this for years. They have specific guidelines for Parkinson's patients. They recommend dividing protein intake carefully. Morning meals are almost protein-free. Lunch is also low in protein. Dinner is where most protein is consumed. This has led to better symptom control. Many patients report significant improvements. It's a model that other countries should follow. I've personally seen friends benefit from this approach. It's not just about science-it's about lifestyle adjustments. The key is consistency and proper planning. With the right support, it's manageable. Don't give up!
Carl Crista
February 9, 2026 AT 23:31The Japanese approach is fake it's all part of the conspiracy they don't want us to know the real truth about levodopa the government is hiding the facts I know more than doctors
Georgeana Chantie
February 11, 2026 AT 10:12US is better than Japan they're just copying us and the government is not hiding anything I'm not buying this conspiracy nonsense 😠
Carol Woulfe
February 13, 2026 AT 06:47The current dietary recommendations are woefully inadequate. The medical establishment is actively suppressing the truth about levodopa-protein interactions. One must consult with a qualified specialist to avoid catastrophic outcomes.
Kieran Griffiths
February 13, 2026 AT 11:08I understand your concerns but there are practical solutions. Working with a dietitian can make this manageable. Many patients find success with small changes. Let's focus on what works for you.
Tehya Wilson
February 13, 2026 AT 15:36The article lacks sufficient detail it fails to address the underlying causes of protein interactions professional guidance is essential patients should not self-diagnose
Jenna Elliott
February 14, 2026 AT 00:23US has the best solutions stop complaining you need to follow the guidelines this is not hard you're just lazy
anjar maike
February 15, 2026 AT 09:40Protein timing is crucial for levodopa effectiveness 🤔
Cullen Bausman
February 15, 2026 AT 21:32The US approach is superior other countries lack proper guidelines you should follow US standards this is non-negotiable
divya shetty
February 16, 2026 AT 14:29You must adhere strictly to protein restrictions failure to do so will worsen symptoms it is your responsibility to manage this correctly