Medicare Part D isn’t just a prescription drug benefit-it’s a massive economic engine built around one simple idea: generics save money. Since its launch in 2006, the program has filled over 10 billion prescriptions. Of those, nearly 9 out of 10 have been for generic drugs. That’s not an accident. It’s the design.
How Medicare Part D Makes Generics the Default Choice
Every Medicare Part D plan uses a tiered formulary-a list of covered drugs sorted by cost. Tier 1 is where you’ll find preferred generics. These are the cheapest options, often with $0 to $10 copays for a 30-day supply. Tier 2 is for non-preferred generics, usually $15-$20. Tier 3 and above? That’s where brand-name drugs live, costing $45 to $100 or more per month.
The system doesn’t just encourage generics-it pushes them. If you pick a brand-name drug when a generic is available, you pay more. If you choose a non-preferred generic, you pay more. The math is clear: go with the lowest tier, save the most.
By 2023, 87.3% of all Part D prescriptions were for generics. That’s up from 55% in 2006. The reason? Plans are required to cover at least two generic drugs in each of 148 common therapeutic categories. That means if you need blood pressure medicine, diabetes pills, or cholesterol drugs, you’ll almost always have at least one low-cost generic option.
The Real Cost Difference: Generics vs. Brand Names
The numbers don’t lie. A 30-day supply of a generic blood pressure drug like amlodipine might cost $0 at a preferred pharmacy. The brand-name version, Norvasc? Around $45. That’s $540 a year saved-just on one pill.
For a Medicare beneficiary taking five medications, switching from brand to generic can cut annual drug spending by $1,500 to $2,500. The Medicare Payment Advisory Commission found that generic drugs cost Part D plans an average of $18.75 per prescription. Brand-name drugs? $156.42. That’s 88% less cost to the program.
And here’s the kicker: even though generics make up 87% of prescriptions, they only account for 24% of total drug spending. Brand-name drugs, at just 13% of prescriptions, make up 76% of the bill. That’s the power of volume and price control.
How the System Keeps Saving Money-Even in the ‘Donut Hole’
For years, Medicare beneficiaries hit a coverage gap called the ‘donut hole.’ Once they spent a certain amount out of pocket, they had to pay full price for drugs until they reached catastrophic coverage. In 2019, beneficiaries paid 70% of the cost for brand-name drugs and 44% for generics in the donut hole.
That changed with the Bipartisan Budget Act of 2018. Now, in the coverage gap, you pay only 25% of the negotiated price-whether it’s a generic or brand-name drug. That’s a huge win for cost-conscious users. And in the catastrophic phase, you pay the greater of 5% coinsurance or a small copay: $4.15 for generics, $10.35 for brands.
That’s not just fair-it’s strategic. By keeping generic copays low even at the highest spending levels, the program makes it financially irrational to choose a brand-name drug unless absolutely necessary.
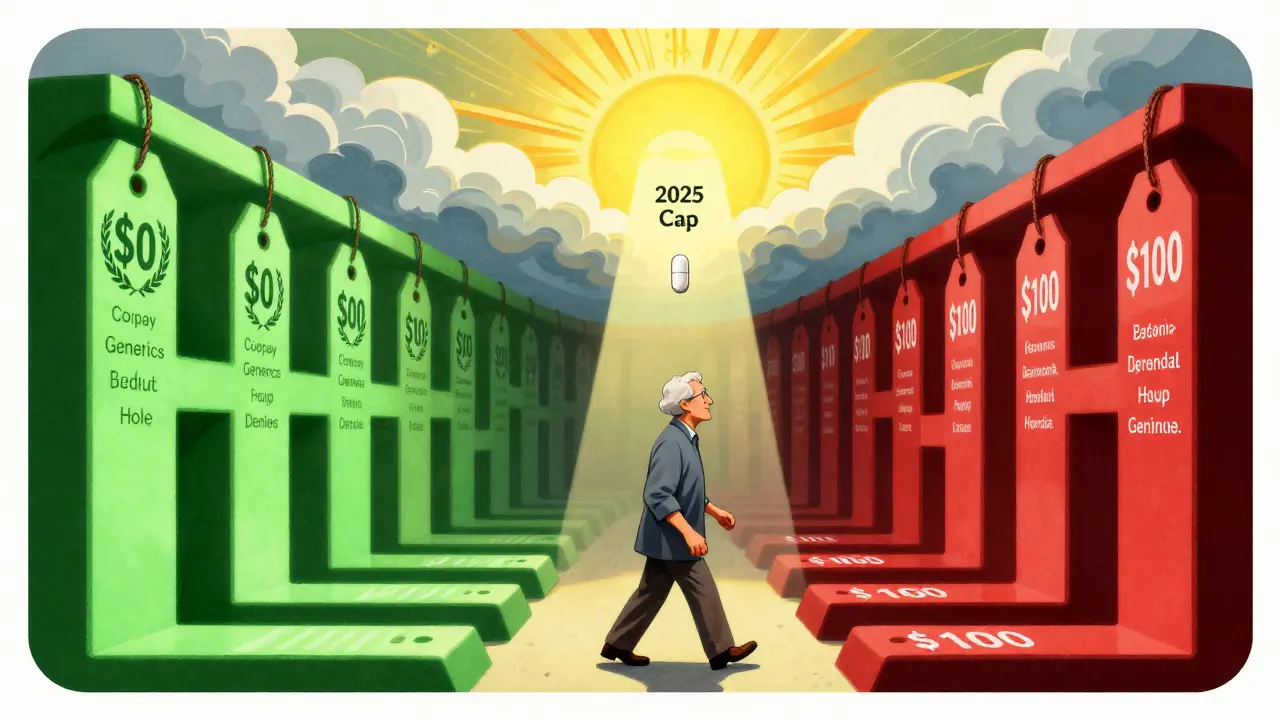
The ,000 Cap and the New Rules That Are Changing Everything
Starting in 2025, there’s a hard cap on out-of-pocket drug spending: $2,000 a year. After that, you pay nothing for the rest of the year. This doesn’t just help people with expensive cancer drugs or rare disease treatments-it helps people taking multiple generics too.
Why? Because if you’re hitting the cap, you’re probably on multiple medications. Generics keep your total spending lower, so you reach the cap faster. Once you’re there, you’re free. The system rewards smart choices.
Also in 2025, manufacturers must give additional discounts on drugs during both the initial coverage phase and the catastrophic phase. This is called the Manufacturer Discount Program. It’s designed to push even more people toward generics. Analysts predict generic use will climb to 91.5% by 2027.
Where the System Still Lets People Down
Generics are cheaper, but they’re not always easy to get. Some plans put a generic drug in Tier 3 just because it’s made by a less popular manufacturer-even if it’s chemically identical to the Tier 1 version. That’s called ‘tier shifting.’ A 2023 CMS report found that 63% of beneficiaries would pay more if they switched plans without checking the formulary.
Another problem: automatic substitution. Pharmacists are allowed to swap a brand for a generic unless the doctor writes ‘dispense as written.’ That’s fine-unless the generic causes side effects. One user on Reddit shared that a generic version of an antidepressant gave them severe dizziness. They had to file a coverage exception to get the brand back. CMS approved 78% of those requests in 2023, but the process takes time.
And then there’s the income gap. Even with generics, 32% of low-income beneficiaries skip doses because they can’t afford even the $10 copay. The $35 monthly cap on insulin helps, but it doesn’t fix everything. Many people still choose between food, rent, and pills.

What You Can Do to Save Money
You don’t have to guess. Use the Medicare Plan Finder tool. It’s free, official, and updated every year during the Annual Enrollment Period (October 15 to December 7). Enter your medications, your pharmacy, and your zip code. It will show you plans with $0 copays for your generics.
Look for plans that cover your drugs in Tier 1. Check if your pharmacy is preferred. Some plans have $0 copays at Walmart or CVS, but $15 at your local pharmacy. That’s $180 a year right there.
If a generic makes you sick, ask your doctor to write ‘dispense as written.’ Then file a coverage determination. You don’t need a lawyer. Just call your plan. They have to respond in 72 hours.
And don’t assume your plan stays the same. Every year, plans change formularies. A drug that was $0 one year might be $25 the next. Check your mail. You’ll get a notice if your drug moves tiers.
Why Generics Are the Backbone of Medicare Part D
The Congressional Budget Office estimates that generic use saves the federal government $14.2 billion every year in subsidies and catastrophic payouts. Since 2006, it’s saved over $1.37 trillion.
That money doesn’t just help the government. It keeps premiums lower for everyone. It lets plans offer $0 copays. It funds the $2,000 out-of-pocket cap. Without generics, Part D would be unaffordable.
But the system isn’t perfect. It’s complex. It’s full of fine print. And it doesn’t always account for how real people live.
Still, if you understand how it works, you can use it to your advantage. Choose the right plan. Know your tiers. Ask questions. And don’t let a $10 copay stop you from getting the medicine you need.
Are generic drugs as effective as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same FDA standards for quality, safety, and effectiveness. The only differences are in inactive ingredients (like fillers or dyes), packaging, and price. For 9 out of 10 people, generics work just as well.
Why do some generic drugs cost more than others?
It’s not about the drug-it’s about the plan. Two identical generic pills can be on different tiers based on which manufacturer the plan negotiated a deal with. A plan might put a generic made by Teva in Tier 1 because they got a bulk discount, but put the same drug made by Mylan in Tier 2. Always check your plan’s formulary, not just the drug name.
Can I switch to a different generic if one causes side effects?
Yes. If a generic causes problems, ask your doctor to prescribe a different generic version of the same drug. Many conditions have multiple generic options. If none work, your doctor can request a coverage exception for the brand-name drug. Medicare approves these requests 78% of the time when supported by medical evidence.
Does the $2,000 out-of-pocket cap in 2025 mean I won’t pay anything for drugs anymore?
No. The $2,000 cap is the most you’ll pay in a year for all your covered drugs. After that, you pay nothing for the rest of the year. But you still have to pay until you hit that cap. Generics help you get there faster because they cost less upfront. If you’re taking mostly generics, you’ll reach the cap sooner and save more in the long run.
Why do some pharmacies charge more for the same generic?
Plans have preferred pharmacies-usually big chains like CVS, Walgreens, or Walmart-that have negotiated lower prices. If you use a non-preferred pharmacy, you pay more. Always check your plan’s pharmacy network. Sometimes, using mail-order or a preferred pharmacy can cut your monthly cost in half.
What if my plan drops a generic I’m taking?
Your plan must give you 60 days’ notice before removing a drug from its formulary. You can request a one-time refill at the old price, or ask for a coverage exception. If you’ve been on the drug for a long time and it works well, your doctor can argue it’s medically necessary. Most exceptions are approved if you show you’ve tried other options or have had bad reactions.
Are there any drugs that don’t have generics?
Yes, but they’re rare. Most drugs have generics after their patent expires. Newer biologic drugs-like some cancer or autoimmune treatments-don’t have true generics yet, but they have ‘biosimilars,’ which are very similar and often cheaper. Part D plans cover biosimilars and encourage their use. If you’re on a brand-name biologic, ask your doctor if a biosimilar is an option.
What Comes Next for Medicare Part D and Generics
The future of Part D depends on one thing: keeping generics cheap and accessible. With the manufacturer discount program, the out-of-pocket cap, and new rules requiring at least one no-prior-auth generic in every category, the system is getting smarter.
But it’s not just about policy. It’s about people. If beneficiaries can’t afford even $5 for a pill, the system fails-even if the math looks perfect. The real success of Part D isn’t measured in billions saved. It’s measured in lives improved because someone didn’t have to choose between their medicine and their rent.





rachel bellet
January 18, 2026 AT 04:02The structural incentives in Part D are a masterclass in behavioral economics-tiered formularies exploit loss aversion and default bias to nudge beneficiaries toward generics. The 88% cost differential between generic and brand-name prescriptions isn’t just fiscal policy; it’s a public health intervention disguised as cost containment. But let’s not pretend this is altruistic. The program’s success is predicated on suppressing pharmaceutical innovation incentives, and the manufacturer discount program in 2025 is just the next phase of price suppression under the guise of consumer protection.
Meanwhile, the $2,000 cap creates a perverse incentive: beneficiaries on high-cost biologics will hit the cap faster, but those on generics will never reach it, meaning the system still disincentivizes adherence for chronic, low-cost conditions. That’s not efficiency-it’s rationing by arithmetic.
Pat Dean
January 19, 2026 AT 12:40They want you to believe generics are just as good, but anyone who’s actually taken them knows better. I tried the generic version of my thyroid med and ended up in the ER with heart palpitations. The FDA says they’re ‘bioequivalent’-whatever that means. Meanwhile, Big Pharma is laughing all the way to the bank while seniors are forced to gamble with their health because the system won’t let them choose what actually works.
This isn’t healthcare. It’s corporate socialism with a side of patient abuse.
Jay Clarke
January 19, 2026 AT 21:32Yo, let’s be real-this whole ‘generics save money’ thing is just a fancy way of saying ‘we’re gonna make you take whatever’s cheapest, even if it makes you feel like a zombie.’
I switched to a generic for my anxiety med and spent three weeks feeling like I was underwater. My doctor had to fight the plan just to get me back on the brand. And yeah, it cost more-but I could breathe again. So don’t tell me about ‘volume and price control’ when your ‘control’ is making people sick.
Generics aren’t the hero. They’re the villain with a $10 copay.
Selina Warren
January 21, 2026 AT 18:57This isn’t just about money-it’s about dignity. Every time someone chooses a generic because they can’t afford the brand, they’re not just saving a few bucks-they’re choosing to live. And that’s powerful.
The system isn’t perfect, but it’s the best we’ve got. The $2,000 cap? That’s hope. The fact that you can now get insulin for $35? That’s justice.
Don’t let the trolls scare you off. Use the Plan Finder. Check your tiers. Call your plan. You have power here. Don’t let them convince you that you’re powerless. You’re not a patient-you’re a consumer with rights. And you deserve to be healthy.
Robert Davis
January 23, 2026 AT 17:11Interesting how the article glosses over the fact that generics aren’t always identical. The inactive ingredients? They can trigger allergies, GI distress, even mood swings. I’ve seen it. My uncle’s generic sertraline gave him panic attacks. The brand didn’t. But the plan forced him into the cheaper version.
And now they’re pushing biosimilars like they’re the same thing. They’re not. They’re just cheaper versions of expensive drugs. It’s not innovation-it’s substitution by bureaucracy.
Also, why is no one talking about how pharmacy benefit managers (PBMs) pocket the difference between what the plan pays and what the pharmacy gets? That’s where the real money is.
Jake Moore
January 24, 2026 AT 14:49For anyone struggling with Part D: use the Medicare Plan Finder. Seriously. I used to pay $42 a month for my generic metformin. Switched plans during AEP, same pharmacy, now it’s $0. No joke.
Also, if your pharmacy charges more than Walmart or Kroger for the same generic, you’re being ripped off. Mail-order is usually cheaper too. And if a generic messes with you? Tell your doctor to write ‘dispense as written’-it’s not hard.
It’s not magic. It’s just knowing how the system works. You don’t need a degree. You just need to ask.
Ryan Otto
January 24, 2026 AT 22:40Let’s not romanticize this. The entire Medicare Part D structure is a state-engineered mechanism to suppress pharmaceutical innovation under the banner of ‘affordability.’ The 9 out of 10 generics statistic is misleading-it reflects regulatory coercion, not market preference.
The manufacturer discount program? A backdoor price control. The $2,000 cap? A fiscal Band-Aid that will inevitably lead to reduced formulary access and increased prior authorization burdens. This is not healthcare reform-it’s economic central planning disguised as benevolence.
And the real beneficiaries? Not patients. Not even taxpayers. The PBMs and large pharmacy chains who negotiate the ‘discounts’ behind closed doors.
Wake up. This is how you lose freedom one copay at a time.
Max Sinclair
January 25, 2026 AT 14:06I appreciate the depth of this breakdown. It’s rare to see a post that doesn’t just rant about drug prices but actually explains how the system works-and how to navigate it.
One thing I’d add: if you’re on multiple generics and hit the $2,000 cap early, you’re not just saving money-you’re buying peace of mind. No more choosing between meds and groceries. That’s huge.
And yes, generics aren’t perfect. But for the vast majority, they’re safe, effective, and life-changing. The real issue isn’t the generics-it’s the inconsistent formularies and lack of transparency. That’s what needs fixing.
Thanks for the clarity. This is the kind of info that actually helps people.
christian Espinola
January 26, 2026 AT 14:47Generics work fine… until they don’t. And when they don’t, you’re stuck in a 30-day appeals process while your blood pressure spikes or your depression worsens.
The system is rigged. PBMs, manufacturers, and CMS all profit from this charade. The ‘savings’ are real-but they come at the cost of patient autonomy.
And don’t get me started on how some plans put the exact same generic on different tiers based on which manufacturer paid the most.
This isn’t healthcare. It’s a casino where your life is the bet.