When your prescription runs out and no pharmacy has it in stock, it’s not just inconvenient-it’s dangerous. Drug shortages aren’t rare exceptions anymore. They’re a growing crisis. In 2025 alone, over 250 different active ingredients were in short supply across the U.S., affecting nearly 2,000 brand-name and generic drugs. Some of these are life-saving: insulin, chemotherapy drugs, antibiotics, even basic pain relievers like injectable acetaminophen. And when they vanish, patients are left scrambling.
Why Are Medications Running Out?
It’s not one single cause. Drug shortages happen because of a mix of broken systems. Manufacturing problems are the biggest culprit-contamination, equipment failure, or quality control failures can shut down a whole production line. For example, a single factory making injectable antibiotics might supply 80% of the country’s needs. If it shuts down for a month, hospitals and pharmacies feel it immediately. Then there’s the business side. Many generic drugs are made by just five companies. If one decides it’s not profitable to keep making a cheap, low-margin drug like amoxicillin, they stop. No one else steps in fast enough. The FDA has stepped up inspections since early 2025, doing monthly checks instead of quarterly, which has cut new manufacturing shortages by 15%. But that’s a band-aid, not a fix. And then there’s supply chain fragility. A raw ingredient from overseas, delayed by shipping or politics, can stall production for months. Even something as simple as a broken pump in a sterile injectable plant can cause a nationwide shortage.What Can You Do When Your Drug Is Unavailable?
Don’t stop taking your medication. Don’t try to stretch doses. Don’t wait until you’re out to act. Here’s what works:- Check the FDA Drug Shortage Database-it’s the most reliable public source. It lists current shortages, expected resolution dates, and sometimes lists therapeutic alternatives. For example, if Semglee (a biosimilar insulin) is out, the database will note that Lantus is an acceptable substitute without needing a new prescription.
- Call multiple pharmacies-not just your usual one. Chain pharmacies like CVS, Walgreens, and Rite Aid often have different stock levels. Mail-order pharmacies might have inventory when local stores don’t. One patient in Texas spent three days calling seven pharmacies before finding Semglee for their child.
- Ask your pharmacist-they’re not just filling scripts. Nearly 90% of major pharmacy chains now have dedicated shortage specialists. They can tell you what’s available, what’s coming in, and whether a substitute is safe.
- Talk to your doctor-not every alternative is a direct swap. For insulin, switching from Semglee to Lantus is straightforward because they’re biosimilar. But switching from one blood thinner to another? That requires dosage changes and monitoring. Your doctor needs to approve any change.
- Check your insurance formulary-just because a drug is available doesn’t mean your plan covers it. During the Semglee shortage, Blue Cross NC removed prior authorization for Lantus on some plans. If you don’t check, you might get stuck with a $500 copay for a substitute that should be covered.
When Substitutions Work (and When They Don’t)
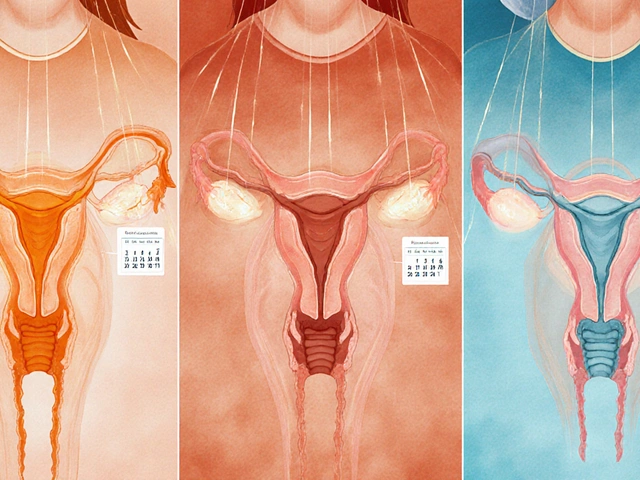
Not all drugs have safe alternatives. Some substitutions are well-established. Others carry real risks. For insulin, biosimilars like Semglee and Lantus are interchangeable. Switching between them doesn’t require a new prescription in many states. That’s a win. But for drugs like alteplase (used in stroke and heart attack treatment), alternatives are limited. Some hospitals started using it for pulmonary embolism during shortages-but that’s off-label use, and outcomes vary by patient. Antibiotics are tricky. When amoxicillin ran low, doctors turned to azithromycin. But azithromycin works differently. It’s not a true substitute-it’s a different class of antibiotic. That means it might not treat the same infection, and overuse increases antibiotic resistance. Oncology drugs are the hardest. Of the 15 cancer medications in shortage between 2023 and 2025, 7 were pediatric chemotherapy agents. There’s often no alternative. Doctors have to delay treatment, reduce doses, or use older, less effective drugs. That’s not a choice-it’s a last resort.
What States Are Doing to Help
Some states are taking action. Hawaii’s Medicaid program now allows foreign-approved versions of drugs during shortages-like a version of insulin approved in Canada or Europe. That’s a bold move. It requires special FDA waivers, but it’s working for patients who can’t get their meds otherwise. New Jersey is considering letting pharmacists dispense emergency insulin supplies without a prescription during shortages. That’s huge. For a parent whose child needs insulin and can’t find any, that could be life-saving. California, New York, and Massachusetts are stockpiling drugs like mifepristone (used in medical abortion) in case federal restrictions cut off supply. It’s not just about shortages-it’s about protecting access. New York is also pushing for a public, searchable database that shows which pharmacies have which drugs in stock. Right now, you have to call every pharmacy. A map showing real-time inventory would change everything.What Patients Are Saying
Reddit threads and patient surveys tell a real story. One user, DiabeticDad87, spent days calling pharmacies for Semglee. Another said they stopped their GLP-1 weight loss medication because they couldn’t get it-and gained back 30 pounds in three months. A Sterling Institute survey found that 68% of patients who talked to their doctor about alternatives had a smooth transition. But 32% stopped taking their meds altogether. That’s the scary part. People don’t know what to do. They think, “If I can’t get it, I’ll just wait.” But for blood pressure meds, seizure drugs, or insulin, waiting can land you in the ER. Some patients reached out directly to manufacturers. Pfizer gave exact timelines for amoxicillin restocks. That helped people plan. Others found help through patient assistance programs or nonprofit organizations that distribute free or low-cost meds during shortages.
What’s Changing in 2025
The good news? Things are starting to shift. Health systems are testing real-time data tools that alert doctors at the moment they write a prescription if the drug is in shortage. Pilot programs at 47 major hospitals cut the time to find alternatives by 28%. That’s faster than calling five pharmacies. The FDA is now monitoring critical drug factories more closely. Manufacturers are starting to diversify their supply chains-though slowly. And more states are passing laws to give pharmacists more authority during shortages. But the big picture hasn’t changed: the system is still built on thin margins, single-source suppliers, and reactive fixes. Without structural changes, shortages will keep happening.What You Can Do Now
You don’t have to wait for policy to fix this. Here’s your action plan:- Know your meds-if you take insulin, blood thinners, or chemotherapy, know what the alternatives are. Ask your pharmacist now, not when you’re out.
- Keep a 30-day supply-if your drug is on the FDA shortage list, ask your doctor if you can get a 90-day prescription. Many insurers allow this for critical meds.
- Use the FDA database regularly-check it monthly. Shortages come and go. A drug that’s available today might be gone next month.
- Connect with patient groups-Reddit, Facebook groups, and disease-specific nonprofits often share real-time info on availability and workarounds.
- Ask your pharmacy for a shortage alert-many now offer text or email alerts when your drug is back in stock.
Drug shortages aren’t going away. But you don’t have to be helpless. With the right steps, you can keep your treatment on track-even when the system fails.
What should I do if my insulin is out of stock?
If your insulin (like Semglee) is unavailable, check the FDA Drug Shortage Database for approved alternatives. Lantus is a biosimilar and often can be substituted without a new prescription. Call multiple pharmacies, including mail-order services. Talk to your doctor to confirm the switch is safe for your condition. Your pharmacist can help you navigate insurance coverage changes during shortages.
Can I use a foreign-approved drug if mine is in short supply?
In some cases, yes. Hawaii’s Medicaid program allows foreign-approved drugs during shortages, but this requires special FDA waivers. Not all states or insurers permit this. Talk to your doctor and pharmacist first. Never import drugs on your own-quality and safety can’t be guaranteed.
Are generic drugs more likely to be in shortage?
Yes. About 85% of generic drugs are made by just five manufacturers. If one company stops production due to low profit margins or a quality issue, the entire market can run out. Generic antibiotics, injectables, and chemotherapy drugs are most at risk.
Can my pharmacist switch my medication without my doctor’s approval?
It depends on the drug and your state. For biosimilars like Semglee and Lantus, pharmacists can substitute without a new prescription in many states. For other drugs, they can’t. New Jersey and other states are pushing laws to let pharmacists dispense emergency insulin without a prescription during shortages-but that’s still new and not universal.
How long do drug shortages usually last?
Many last over a year. Between 2018 and 2023, 75% of drug shortages lasted more than 12 months, and 58% lasted two years or longer. Chronic shortages are common for sterile injectables, chemotherapy drugs, and essential generics. Don’t assume it’ll be resolved quickly.
Is it safe to split pills or stretch my dose if I’m running low?
No. For drugs like blood thinners, seizure medications, or insulin, even small changes in dose can be dangerous. Splitting pills can lead to inaccurate dosing. Stretching doses may cause your condition to worsen. Always consult your doctor before making any changes to your regimen.




James Rayner
December 16, 2025 AT 19:52It’s heartbreaking, really… I’ve watched my dad go through this with his insulin. Not because he’s lazy or careless-but because the system is broken. One factory. One machine. One quality control slip. And suddenly, a life-saving drug vanishes like it was never meant to exist. We called seven pharmacies. Three said ‘maybe next week.’ One had it-but the price was triple. I sat in the car for 45 minutes crying before I called the doctor. It’s not just about access-it’s about dignity. We shouldn’t have to beg for the right to live.
And yeah, I know the FDA’s trying. But when your child’s life depends on a spreadsheet update, you start to wonder if ‘trying’ is enough.
😭
Dave Alponvyr
December 18, 2025 AT 13:55So… you’re telling me we’re all just supposed to call 7 pharmacies and hope for the best? Wow. Real innovative. I’m sure the guy on chemo is just thrilled he gets to play pharmacy roulette while his immune system tanks.
Meanwhile, the CEOs are sipping champagne on their yachts. 🍾
Joanna Ebizie
December 20, 2025 AT 06:27Ugh. People still don’t get it. This is all because we let big pharma run wild. You think they’re making less profit on generics? Nah. They’re just waiting for you to panic so they can jack up the price on the ‘alternatives.’
And don’t even get me started on ‘biosimilars.’ That’s just corporate speak for ‘we made a copy that’s 95% the same but we’re charging you the same price.’
Stop being so nice to the system. It’s rigged.
Also, if you’re still using Walmart’s $4 insulin, you’re lucky. Most people aren’t.
🙄
Elizabeth Bauman
December 21, 2025 AT 09:41Let me tell you something-this isn’t an accident. This is deliberate. The FDA? They’re controlled. The supply chain? Manipulated. Why do you think every single antibiotic shortage happens right after a new vaccine rollout? Coincidence? NO.
They want you dependent on their ‘alternatives’-the ones made in China or India with questionable ingredients. And now they’re pushing ‘foreign-approved’ drugs like it’s a solution? HA. That’s just the first step to letting in cheap, unregulated meds from countries that don’t even have FDA standards.
Remember when they said 5G was harmless? Now look at us. We’re being slowly poisoned by the same people who promise to ‘protect’ us.
Check your formulary. Check your pharmacy. Check your soul. This is stage one of the Great Medication Takeover.
🇺🇸 #WakeUpAmerica
Dylan Smith
December 22, 2025 AT 23:12So if I’m on blood thinners and my drug’s out what do I do exactly
Do I just stop until someone tells me what to take
And who decides what’s safe
Why does my doctor need to approve everything but the pharmacy can’t even tell me if it’s in stock
And why is this even allowed to keep happening
It’s not like we’re talking about fancy skincare here
These are drugs that keep people alive
And no one’s doing anything
Just saying
Mike Smith
December 23, 2025 AT 21:56Thank you for this comprehensive and deeply necessary overview. The systemic vulnerabilities exposed here are not merely logistical-they are moral failures of our healthcare infrastructure.
It is both commendable and deeply concerning that patients are being forced to become supply chain analysts, insurance navigators, and clinical decision-makers simply to maintain baseline health.
While individual actions-checking the FDA database, contacting pharmacists, securing 90-day fills-are prudent and necessary, they are not sustainable solutions. What we require is structural reform: mandatory multi-sourcing for critical medications, federal stockpiling of essential generics, and regulatory incentives for manufacturers to maintain redundant production capacity.
Let us not mistake resilience for justice. We must demand more than survival. We must demand dignity.
With profound respect,
Mike Smith, RN, MSN
Kitty Price
December 23, 2025 AT 23:46My mom had to switch from one blood pressure med to another last year during a shortage. She was fine. But she cried for three days because she was scared.
Just… don’t wait until you’re out. Talk to your pharmacist now. Seriously.
❤️
Colleen Bigelow
December 24, 2025 AT 08:22Oh, so now we’re supposed to be grateful because the FDA ‘cut new shortages by 15%’? That’s like saying ‘we stopped drowning 15% of the people in the ocean.’
And don’t get me started on these ‘foreign-approved’ drugs. You want to hand our children’s insulin over to some factory in Mumbai or Beijing that doesn’t even speak English? That’s not a solution-that’s surrender.
Real Americans don’t take meds from foreign regimes. We have the technology. We have the factories. We have the brainpower.
So why are we letting this happen?
Because the elites don’t care. They’re on brand-name drugs with no copay.
And if you think this is about ‘profit margins’-you’re not thinking big enough.
This is a war. And they’re winning.
🇺🇸 #MakeMedicationsGreatAgain