What to Do Right Now If Your Medicine Is Recalled
Imagine opening your medicine cabinet and seeing a notice: your prescription has been recalled. Your first thought might be to stop taking it-right away. But that’s often the worst thing you can do. Medication recalls happen more often than most people realize. In 2022 alone, nearly 5,000 drugs were pulled from shelves in the U.S., mostly because of manufacturing errors, wrong labels, or tiny bits of contamination. But here’s the truth: 95% of these recalls aren’t emergencies. Most are precautionary. Still, if your medicine is on the list, you need to act-quickly and correctly.
Don’t Stop Taking Your Medicine
Stopping your medication cold turkey can be dangerous. If you’re on blood pressure pills, diabetes meds, or antidepressants, skipping doses can cause serious problems-higher risk of stroke, blood sugar spikes, or even seizures. The FDA made this crystal clear during the 2018 valsartan recall: "Continue taking your medicine until your doctor or pharmacist gives you a replacement." That advice still holds today. A recalled drug might have a tiny impurity, but it’s not suddenly toxic. The real danger? Going without treatment.
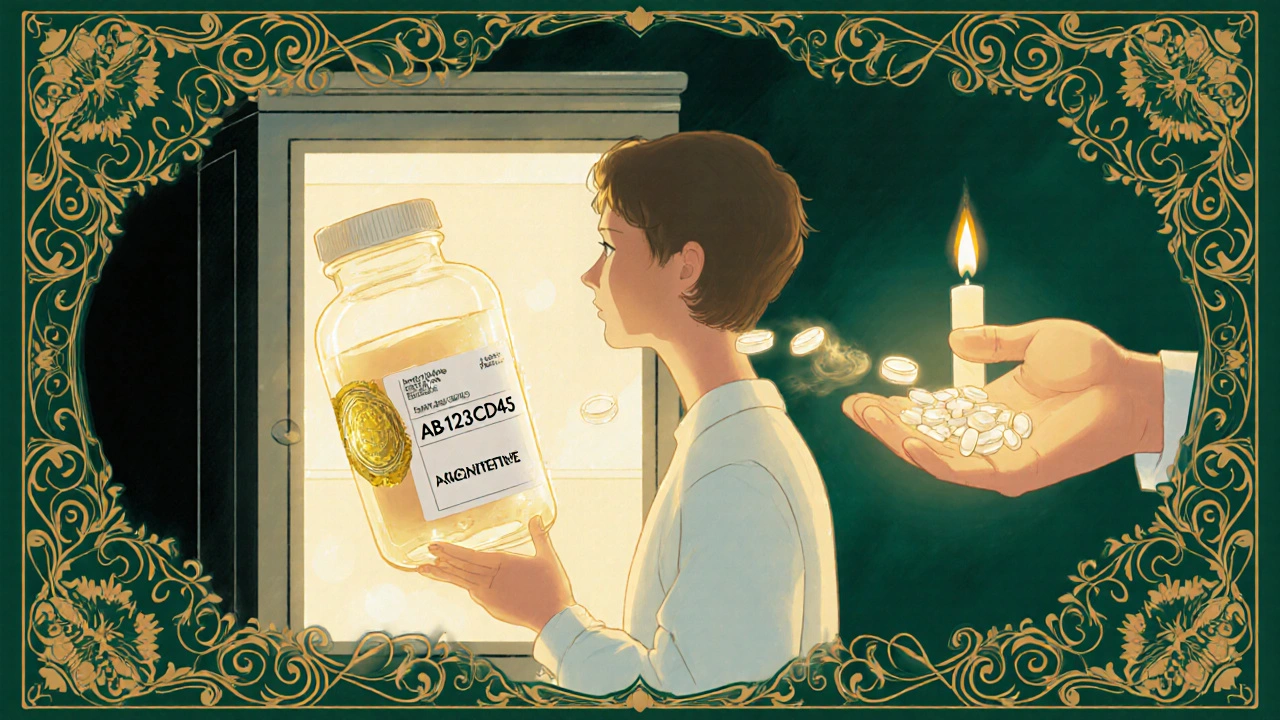
Check Your Lot Number-Not Just the Name
Not every bottle of a recalled drug is affected. Only specific batches, identified by lot numbers, are recalled. You might have the same medicine as someone else, but if your lot number doesn’t match, you’re safe. Look at the label on your bottle. You’ll see a string like AB123CD45 or NDC 0078-9012-34. Compare it to the FDA’s recall notice. If you’re unsure, don’t guess. Call your pharmacy. Pharmacists have systems that flag recalled lots automatically. In fact, 92% of U.S. pharmacies can confirm whether your exact bottle is affected within minutes.
How to Find Out If Your Medicine Is Recalled
The FDA’s website is the only official source you need. Go to www.fda.gov/safety/recalls. Here’s how to search correctly:
- Type in the brand name (like "Lisinopril") or generic name.
- Use the "Product Type" filter to select "Human Prescription Drug".
- Click on the recall notice that matches your drug.
- Check the list of affected lot numbers and expiration dates.
Don’t rely on news headlines or social media. They often get details wrong. The FDA also offers a free RSS feed that sends real-time alerts to your email or phone-45% of healthcare workers use it. If you’re on a long-term medication, sign up. It takes 30 seconds.
What to Do If Your Medicine Is Recalled
Once you confirm your bottle is affected, follow these steps:
- Contact your pharmacy immediately. They’ll check if they have a safe replacement in stock. Most can give you a new bottle within 24 hours.
- Ask your doctor if you need a different drug. Sometimes, switching to another brand or generic is better than waiting.
- Don’t throw it away yet. Wait for instructions. Some recalls ask you to return the medicine to the pharmacy. Others tell you to dispose of it.
If you can’t reach your pharmacy right away, call your doctor’s office. Many have nurses on call for exactly this situation.
How to Safely Dispose of Recalled Medication
When you’re told to throw it out, don’t flush it or toss it in the regular trash. That’s unsafe for kids, pets, and the environment. The FDA recommends this method:
- Take the pills out of the bottle.
- Mix them with something unappetizing-used coffee grounds, cat litter, or dirt.
- Put the mixture in a sealed plastic bag or container.
- Throw it in the trash.
Some pharmacies offer take-back bins. Ask if yours does. If the recall notice gives different instructions, follow those instead. If it’s unclear, call your pharmacist. They’ve done this before.
Watch for Side Effects-And Report Them
Even if you took the recalled medicine for weeks without issues, keep an eye out. Some side effects show up slowly. If you feel dizzy, nauseous, unusually tired, or have strange rashes, call your doctor. Write down when you took the medicine, what dose, and when symptoms started. This info helps doctors and the FDA track patterns.
The FDA’s MedWatch program lets patients report bad reactions directly. In 2022, over 140,000 reports came from people like you-and 27% of those led to new recalls. Your report could prevent someone else’s harm.
What Most People Get Wrong
Studies show the biggest mistakes patients make:
- Stopping meds too soon (22% of cases-this causes more hospital visits than the recall itself).
- Assuming all bottles are bad (45% of people skip checking lot numbers).
- Flushing pills (30% still do this, even though it’s unsafe).
Don’t be one of them. A recall isn’t a panic signal. It’s a call to verify, then act.
Be Prepared for Next Time
Most people don’t track their meds beyond the bottle. But keeping a simple log saves hours-and maybe your health. Write down:
- Drug name (brand and generic)
- Dosage
- Lot number
- Expiration date
- Pharmacy name
Keep it in your phone notes or a small notebook. The National Community Pharmacists Association found that patients who do this resolve recalls 60% faster than those who don’t. In a crisis, that’s priceless.
Why Recalls Are Increasing
Recalls are up 12% since 2021. Why? Global supply chains are more complex. A single ingredient might come from three countries before it’s made into a pill. That’s more chances for errors. The most commonly recalled drugs in 2022 were blood pressure medications (like valsartan), diabetes drugs, and cancer treatments. The FDA is improving its digital alerts-new systems now push recall notices directly to pharmacy systems, so patients get notified faster. Pilot programs show patients respond 35% quicker when they’re alerted through their pharmacy app or online portal.
Class I, II, III: What the Levels Mean
Not all recalls are equal. The FDA classifies them:
- Class I (15% of recalls): Highest risk. Could cause serious injury or death. Requires immediate action.
- Class II (70%): Might cause temporary or reversible harm. Still needs attention.
- Class III (15%): Unlikely to cause harm. Usually just a labeling error.
When you see a recall notice, check the class. If it’s Class I, call your pharmacist within hours. If it’s Class III, you can wait a day. But always verify your lot number-don’t assume.
What should I do if I’ve already taken a recalled medicine?
If you’ve taken the recalled medicine, don’t panic. Most recalled drugs don’t cause immediate harm. But monitor yourself for unusual symptoms like dizziness, nausea, rash, or extreme fatigue. Write down when you took it and any changes you notice. Call your doctor if you’re concerned. Even if you feel fine, it’s smart to get a replacement from your pharmacy to avoid future exposure.
Can I get a refund or replacement for a recalled drug?
Yes. Your pharmacy will replace the recalled medication at no cost, even if you’ve used some of it. Most insurance plans cover the replacement. If you’re paying out-of-pocket, the manufacturer typically covers the cost. Ask your pharmacist-they’ll handle the paperwork. You don’t need to file a claim yourself.
What if my pharmacy doesn’t have a replacement?
If your pharmacy doesn’t have a replacement, ask them to order it from another supplier. Most can get it within 24-48 hours. If you’re on a chronic medication and the delay is longer, your doctor can prescribe a similar drug from a different manufacturer. Never go without treatment. The FDA advises that the risk of stopping your medicine is often greater than the risk of the recalled batch.
Are generic drugs more likely to be recalled than brand names?
No. Generic and brand-name drugs are held to the same safety standards. Recalls happen because of manufacturing issues, not because a drug is generic. In fact, most recalls affect both brand and generic versions made by the same company. Always check the lot number, regardless of the brand.
Should I keep my old medicine bottle after a recall?
Yes-until you’ve confirmed the replacement is safe and you’ve disposed of the recalled batch. The bottle has your lot number, expiration date, and pharmacy info, which you might need for records or if you have to report side effects. Once you’re sure the recall is resolved, you can safely recycle the empty bottle (remove the label first).
Final Reminder: Stay Calm, Stay Informed
Medication recalls sound scary, but they’re a sign the system is working. The FDA and pharmacies catch problems before they hurt people. Your job isn’t to panic-it’s to verify, act, and stay informed. Keep your meds logged. Know your lot numbers. Call your pharmacist. And never stop a medicine without talking to someone who knows your health history. That’s how you protect yourself-not by fear, but by smart, simple steps.




Nikki C
November 24, 2025 AT 04:35Vineeta Puri
November 25, 2025 AT 11:04Victoria Stanley
November 26, 2025 AT 08:34Andy Louis-Charles
November 28, 2025 AT 04:12Douglas cardoza
November 29, 2025 AT 01:13Adam Hainsfurther
November 29, 2025 AT 23:40Rachael Gallagher
December 1, 2025 AT 09:18steven patiño palacio
December 2, 2025 AT 10:16stephanie Hill
December 4, 2025 AT 04:09Akash Chopda
December 5, 2025 AT 01:54Alex Dubrovin
December 6, 2025 AT 16:36Jacob McConaghy
December 7, 2025 AT 07:00Natashia Luu
December 8, 2025 AT 11:54akhilesh jha
December 10, 2025 AT 02:24Jeff Hicken
December 11, 2025 AT 10:49