More than 40% of adults in the U.S. take medications that can react dangerously with alcohol-yet most don’t know it. You might think having a glass of wine with your painkiller or a beer after your antibiotic is harmless. But the truth? Even one drink can turn a safe medication into a health risk. This isn’t about scare tactics. It’s about facts you need to live safely.
How Alcohol Changes How Your Medication Works
Alcohol doesn’t just make you feel drunk. It changes how your body processes medicine. Your liver uses special enzymes-like CYP2E1 and CYP3A4-to break down both alcohol and most prescription drugs. When you drink, these enzymes get busy with alcohol first. That means your medication doesn’t get broken down the way it should.If you drink right after taking a pill, your body might hold onto too much of the drug. That can lead to dizziness, extreme sleepiness, or even breathing problems. On the other hand, if you drink regularly over weeks, your liver starts making more enzymes to handle the alcohol. That speeds up how fast your body clears the medication-so it stops working as well.
Think of it like traffic. Your liver is a busy intersection. Alcohol and medication are two cars trying to get through at the same time. One blocks the other. Sometimes the car (medication) gets stuck. Sometimes it’s forced through too fast. Either way, something breaks.
Medications That Are Especially Dangerous With Alcohol
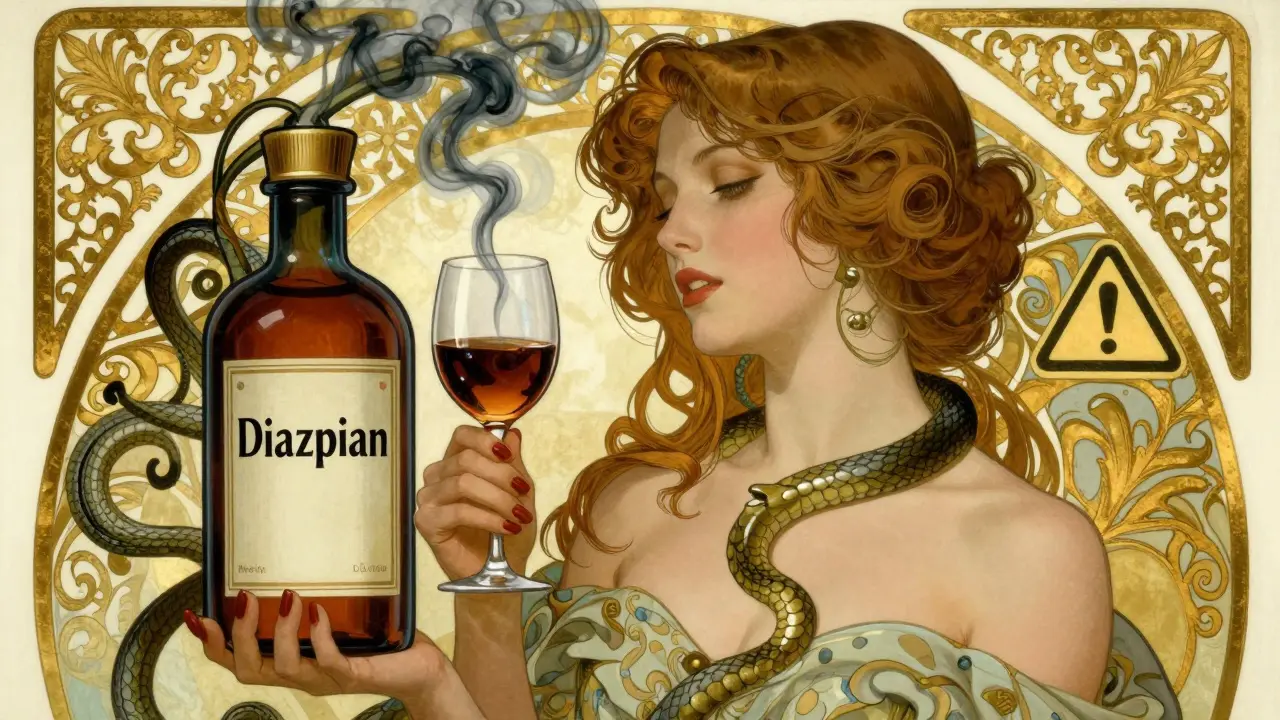
Some medicines mix with alcohol like gasoline and a spark. Here are the biggest risks:- Benzodiazepines (like diazepam, alprazolam): These are sedatives for anxiety or sleep. Alcohol adds to their effect. Together, they can slow your breathing to dangerous levels-even at low alcohol levels like 0.05%. This combination causes over a third of all alcohol-medication deaths.
- Opioids (like oxycodone, morphine): These already depress breathing. Alcohol makes that risk 8 times worse. The CDC says this mix is one of the leading causes of accidental overdose deaths.
- Antibiotics (especially metronidazole and tinidazole): Drinking even one drink with these can trigger a severe reaction-flushing, vomiting, racing heart, chest pain. In 92% of cases, it happens within minutes.
- Antidepressants (like fluoxetine, sertraline): Alcohol makes you feel more drunk and can worsen depression. Studies show it extends how long you feel intoxicated by over three hours.
- Antihistamines (like diphenhydramine): Found in sleep aids and cold meds, these make you sleepy. Alcohol triples that effect. You might fall asleep driving or forget to breathe while sleeping.
- Acetaminophen (Tylenol): Taking more than three drinks a day while using this common painkiller can cause sudden liver failure. Even one drink daily with regular use increases liver enzyme levels in nearly half of users.
- NSAIDs (like ibuprofen, naproxen): These already irritate your stomach. Alcohol adds to that. Together, they raise your risk of internal bleeding by 300-500%.
What ‘Moderate’ Drinking Really Means
Most people think ‘moderate’ means one or two drinks a day. That’s what the guidelines say. But with medication, moderate doesn’t mean safe.Here’s what a standard drink actually is:
- 12 ounces of beer (5% alcohol)
- 5 ounces of wine (12% alcohol)
- 1.5 ounces of spirits (40% alcohol)
That’s it. No tall glasses. No craft cocktails with extra shots. Just these amounts. Even one of these with a high-risk medication can be dangerous.
And timing matters. If you take a medication with a long half-life-like diazepam, which stays in your system for up to 100 hours-waiting until the next day isn’t enough. You might need to wait five to ten days after your last dose before drinking.
What You Should Do Right Now
You don’t need to quit alcohol forever. But you do need to be smart.- Check every new prescription. Ask your doctor or pharmacist: ‘Can I drink alcohol with this?’ Don’t assume it’s fine.
- Read the medication guide. Most come with a printed sheet. Look for words like ‘avoid alcohol,’ ‘may cause drowsiness,’ or ‘risk of liver damage.’
- Use a reliable tool. WebMD and GoodRx have interaction checkers. But be careful-only 37% of online tools are fully up to date. Always cross-check with your pharmacist.
- Know your meds. If you take five or more medications, your risk goes up fast. Keep a list. Show it to your pharmacist every time you fill a new prescription.
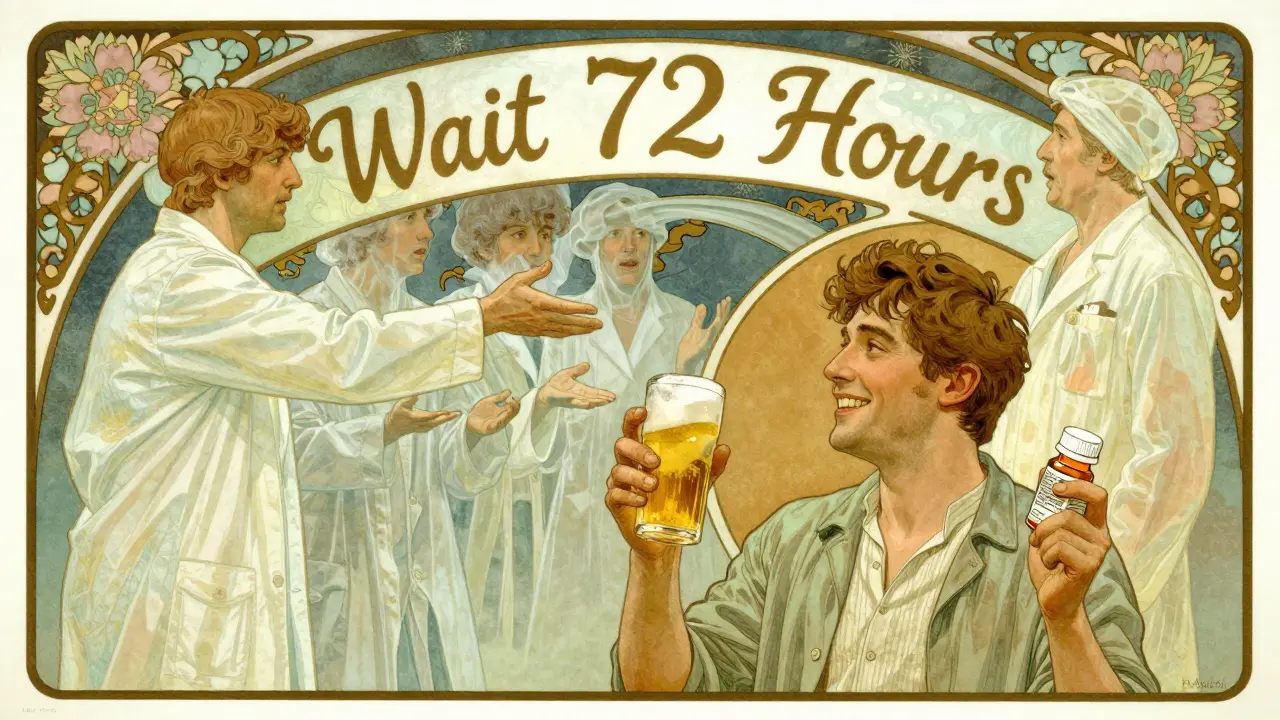
- Wait 72 hours. For high-risk drugs like metronidazole, don’t drink for three full days before and after treatment.
- If you drink, eat first. Food slows alcohol absorption. That gives your liver more time to process both alcohol and medication.
Why Your Doctor Might Not Tell You
It’s not that doctors are hiding this. It’s that they’re overwhelmed. A 2022 survey found 68% of patients say they were never warned about alcohol interactions. Why?Doctors have 15 minutes per visit. They’re focused on your main issue-diabetes, high blood pressure, anxiety. Alcohol might not even come up. And only 42% of prescription bottles have clear alcohol warnings on the label.
Pharmacists, on the other hand, are trained for this. Walgreens data shows 89% of patients changed their drinking habits after a pharmacist gave them a simple warning. That’s why you should always ask your pharmacist when you pick up a new script.
Real Stories, Real Risks
One woman took metronidazole for a bacterial infection. She had one glass of wine at dinner. Within 20 minutes, she was vomiting, her heart was racing at 180 beats per minute, and she ended up in the ER. She didn’t know the warning existed.A man on oxycodone for back pain had a couple of beers after work. He fell asleep on the couch and didn’t wake up. His family found him with shallow breathing. He survived-but barely.
Another patient, on fluoxetine for depression, drank wine every night. He felt more depressed, more tired, and more isolated. His doctor didn’t ask about alcohol. He didn’t think it mattered. Only after his therapist brought it up did he stop-and his mood improved in weeks.
These aren’t rare. They’re common. And they’re preventable.
What’s Changing in 2026
New rules are coming. Starting in 2024, the FDA now requires pictograms on high-risk medication labels-simple icons showing a glass with a red slash. By the end of 2024, Medicare Part D plans must flag prescriptions that interact with alcohol before they’re filled.Telehealth apps now screen for alcohol use during online visits. If you say you drink, the system might pause the prescription until you talk to a pharmacist.
And a new tool called the Alcohol-Medication Interaction Risk Calculator (AMIRC) is being rolled out in clinics. It asks about your age, liver health, how much you drink, and what meds you take-and gives you a personalized risk score.
Bottom Line: Be the Boss of Your Health
You’re not being paranoid. You’re being smart. Alcohol isn’t just a social drink. When it’s in your system with medicine, it becomes a hidden variable that can turn treatment into danger.You don’t have to give up everything. But you do need to know which meds are off-limits. Ask. Read. Check. Wait. If you’re unsure, skip it. One drink isn’t worth a trip to the hospital-or worse.
Your body is working hard to keep you healthy. Don’t make it fight a battle it didn’t sign up for.
Can I have one drink with my prescription?
It depends on the medication. For some, like metronidazole or opioids, even one drink is dangerous. For others, like SSRIs or NSAIDs, one drink might be okay-but only if you’re healthy, don’t drink often, and take the medication as directed. Always check with your pharmacist. Never assume it’s safe.
What if I forgot and had a drink?
If you took a high-risk medication like an opioid or benzodiazepine and drank alcohol, watch for extreme drowsiness, slow breathing, confusion, or loss of coordination. If you feel any of these, call 911 or go to the ER. For less risky meds like ibuprofen or a low-dose antidepressant, you’re likely fine-but avoid another drink and talk to your pharmacist about it.
Does alcohol affect all medications the same way?
No. Some medications are metabolized by the same liver enzymes as alcohol, which causes direct interference. Others affect the same part of the brain-like sedatives-and alcohol just adds to their effect. Some, like antibiotics, trigger chemical reactions that cause sudden, painful symptoms. The risk varies by drug, dose, and how often you drink.
Are over-the-counter drugs safe with alcohol?
Not always. Cold and sleep meds often contain diphenhydramine or acetaminophen-both dangerous with alcohol. Even aspirin or ibuprofen can increase stomach bleeding when mixed with regular drinking. Always read the label. If it says ‘may cause drowsiness’ or ‘do not use with alcohol,’ take it seriously.
Why do older adults face higher risks?
As we age, our liver processes alcohol and drugs more slowly. Blood flow to the liver drops by about 35% between ages 25 and 75. That means alcohol and medications stay in the system longer, increasing side effects. Older adults also take more medications-sometimes five or more-which multiplies interaction risks. The American Geriatrics Society lists 17 high-risk drugs for seniors.
Can I drink the day after taking a medication?
It depends on the half-life. For short-acting drugs like acetaminophen or ibuprofen, waiting 24 hours is usually enough. But for long-acting ones like diazepam or fluoxetine, the drug can still be in your system for days. If you’re unsure, wait 72 hours. When in doubt, skip it.
Is non-alcoholic beer safe?
Most non-alcoholic beers still contain up to 0.5% alcohol. That’s not enough to get you drunk-but it can still trigger reactions with certain drugs like metronidazole. If you’re on a medication with a strict no-alcohol warning, avoid even non-alcoholic beer. Choose sparkling water instead.



Andrew Rinaldi
January 20, 2026 AT 11:56It’s wild how we treat alcohol like it’s harmless just because it’s legal. I used to think one glass of wine with my antidepressant was fine-until I started feeling like a zombie by 8 p.m. Turns out, my brain was just drowning in serotonin and ethanol. Now I wait 72 hours. Not because I’m scared, but because I respect my body more than I respect my habits.
People say ‘it’s just one drink,’ but one drink can be the one that breaks you. And no one warns you until it’s too late.
Pharmacists are the real MVPs here. I’ve learned more from them in five minutes than from my doctor in three years.
Samuel Mendoza
January 20, 2026 AT 22:16You’re all overreacting. One drink won’t kill you. Stop fearmongering.
Glenda Marínez Granados
January 21, 2026 AT 05:32Oh honey, if your liver can’t handle a glass of wine and a pill, maybe it’s time to stop pretending you’re a grown-up.
Also, I’m pretty sure my cat drinks more responsibly than half the people on this thread. 🐱🍷
Yuri Hyuga
January 22, 2026 AT 14:13This is one of the most important pieces of health literacy I’ve read in years. Thank you for breaking it down with such clarity.
Alcohol isn’t the enemy-but ignorance is. And the fact that 68% of patients are never warned? That’s a systemic failure.
I’ve shared this with my entire family. My mom is on five meds, my brother takes oxycodone for chronic pain, and my sister drinks wine every night with her Zoloft. This could save lives.
Let’s push for mandatory pharmacist consultations at pickup. Not just for opioids-for everything. We owe it to each other.
And yes, non-alcoholic beer? Still risky. Sparkling water with lime is the new cool. 🍋
MARILYN ONEILL
January 24, 2026 AT 03:46Ugh. I knew this was gonna be one of those posts. Like, who even drinks anymore? Everyone’s so paranoid. It’s just alcohol. It’s not poison. My grandma drank whiskey with her blood pressure meds and lived to 98.
Also, why are we listening to pharmacists? They just want to sell you more stuff. My doctor said it was fine. End of story.
Coral Bosley
January 25, 2026 AT 19:59I used to drink two glasses of wine every night with my fluoxetine. Thought it helped me relax. Turns out, I was just drunk and depressed at the same time. Like a sad, sluggish zombie with a wine glass.
Stopped. Three weeks later, I felt like I’d been asleep for ten years and finally woke up. My therapist said it was like removing a thick fog from my brain.
Don’t wait for an ER visit. Just stop. Your future self will thank you.
And yes, I cried. A lot. But it was worth it.
Steve Hesketh
January 26, 2026 AT 18:06Brother, I come from a village where every elder says alcohol is medicine. We used to mix local brew with painkillers for backaches. No one died. But I read your post and I realized-we were lucky, not smart.
Now I tell my cousins: ‘If your medicine says no alcohol, then no alcohol. Even if your uncle drank it for 40 years and still dances at weddings.’
Health is not luck. It’s discipline. And discipline is love for yourself.
Thank you for writing this. I’m printing it out and giving copies to my whole family.
God bless you.
shubham rathee
January 26, 2026 AT 23:00Did you know the FDA only started requiring those pictograms because of a lobbying group funded by Big Pharma? The real reason they’re pushing this is to make people dependent on their expensive new drugs that ‘counteract’ alcohol interactions. Also, alcohol is a natural depressant and has been used for centuries. The real danger is the 300% increase in pharmaceutical sales since 2010
Also your liver is fine
And why do you think your doctor doesn’t tell you? Because they’re paid by the system to keep you sick
Also I’ve been on 12 meds and I drink daily and I’m 34 and I run marathons so your science is wrong
Also non alcoholic beer is fine I checked the label
And I’m not paranoid I’m informed
MAHENDRA MEGHWAL
January 28, 2026 AT 11:11Thank you for this comprehensive and meticulously researched exposition. The integration of pharmacokinetic principles with real-world clinical outcomes is both scientifically rigorous and profoundly human.
It is deeply concerning that healthcare systems, particularly in high-income nations, continue to deprioritize patient education on drug-alcohol interactions despite overwhelming evidence of morbidity and mortality risk.
I have shared this with my colleagues in the Department of Clinical Pharmacology at the University of Delhi. We are currently drafting a policy brief to advocate for mandatory pharmacist-led counseling at the point of dispensation for all psychotropic and hepatotoxic medications.
May this post serve as a catalyst for systemic reform.