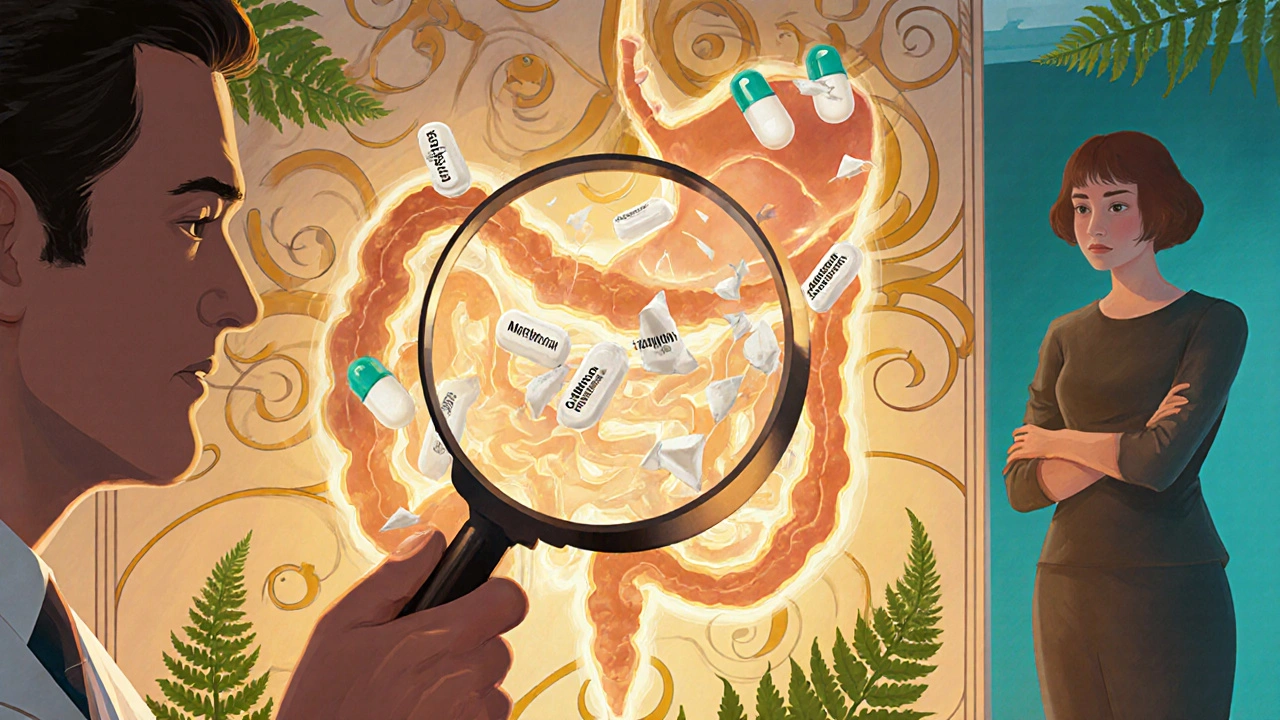
After bariatric surgery, many patients are shocked when their medications stop working the way they used to. A pill that once kept blood pressure under control now seems useless. Thyroid medication no longer regulates energy levels. Painkillers don’t last through the day. This isn’t in their head-it’s physics, chemistry, and anatomy working against them. Bariatric surgery doesn’t just shrink your stomach; it rewires how your body absorbs every single drug you take.
Why Your Pills Don’t Work Like They Used To
Bariatric surgery changes the entire path food-and medication-takes through your digestive system. The most common procedures, sleeve gastrectomy and Roux-en-Y gastric bypass (RYGB), cut the stomach down to a small pouch and reroute the small intestine. That means drugs don’t get the same exposure to acid, enzymes, or surface area they did before.Before surgery, your stomach had a pH between 1.5 and 3.5-strong enough to break down most pills. After surgery, especially with RYGB, that pH rises to 4.0-6.0. That’s the difference between vinegar and lemon juice. Many medications need that acidic environment to dissolve. Enteric-coated pills, designed to survive stomach acid and release in the intestine, often dissolve too early or not at all. Extended-release tablets rely on slow movement through the gut to release medication over hours. After surgery, things move too fast. The stomach empties in 30-60 minutes instead of 2-5 hours. The drug zips through the bypassed section of intestine before it can be absorbed.
One patient, post-RYGB, reported taking his 500mg metformin ER daily and still having high blood sugar. His pharmacist found his plasma levels were only 40% of what they should be. He switched to immediate-release metformin, taken three times a day, and his glucose dropped into target range within two weeks.
Not All Surgeries Are the Same
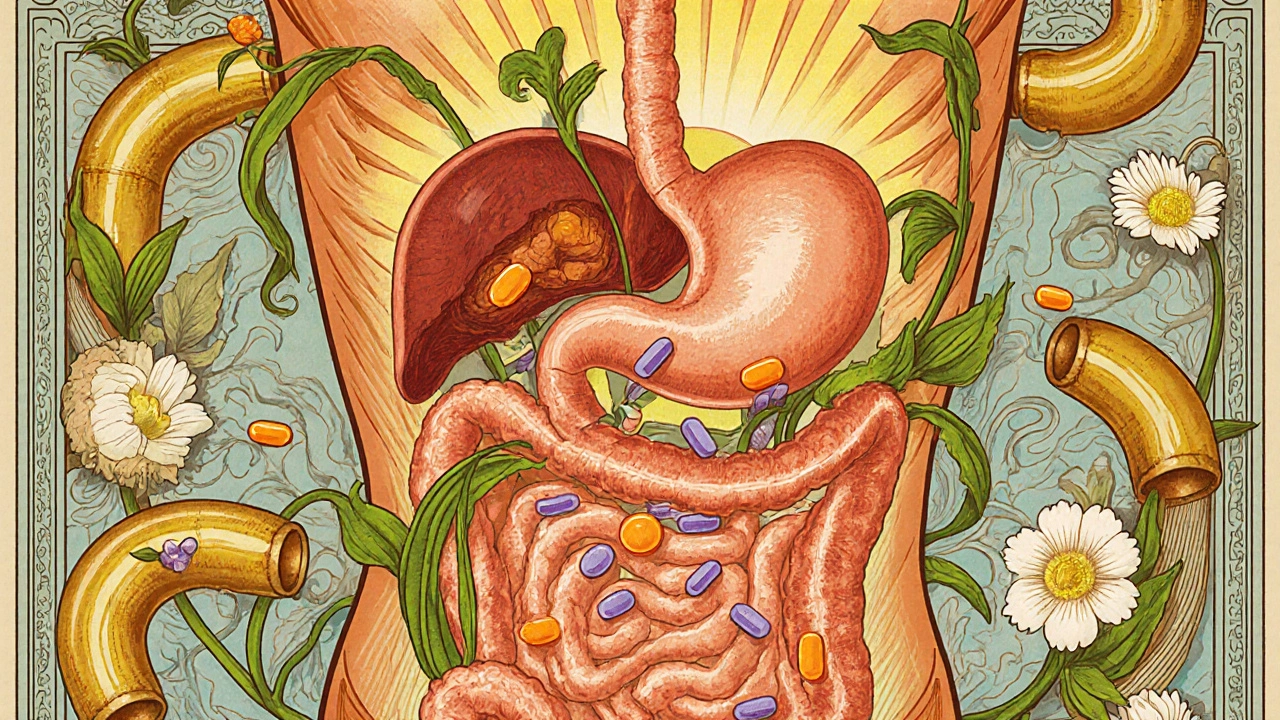
The type of surgery you had makes a huge difference in how your meds behave.- Sleeve gastrectomy removes 80% of the stomach but leaves the intestines intact. Gastric pH rises, and the small pouch can’t hold large pills. Tablet disintegration suffers, but absorption overall drops by only 15-20% for most drugs.
- Roux-en-Y gastric bypass bypasses the duodenum and part of the jejunum-the main absorption zones for many drugs. This causes major drops in absorption for calcium (35% less), levothyroxine (25-30% less), and extended-release drugs like glipizide XL or oxycodone CR (up to 60% less effective).
- Biliopancreatic diversion with duodenal switch is the most extreme. It bypasses nearly 70% of the small intestine. Bioavailability for many drugs drops by 50-70%. This procedure is rare (only 2.5% of cases), but the impact is severe.
- Gastric banding has minimal effect on absorption since the digestive tract isn’t rerouted. But because patients eat so little, food-dependent drugs like mycophenolate mofetil may need higher doses to compensate for low food intake.
The key difference? If your duodenum is bypassed, your body loses its primary site for absorbing iron, calcium, vitamin B12, and many medications. If it’s still in the path, like with sleeve surgery, absorption stays mostly normal.
Drugs That Are Most at Risk
Some medications are especially vulnerable after bariatric surgery. Here’s what you need to watch:- Levothyroxine: Thyroid hormone replacement is absorbed in the upper small intestine. After RYGB, patients often need 20-50% higher doses. One study found 41% of patients needed dose increases within six months.
- Warfarin: This blood thinner has a narrow safety window. Too little, and you risk clots. Too much, and you bleed. After RYGB, 60% of patients need dose increases of 25-35%. Therapeutic monitoring is mandatory.
- Extended-release medications: Metformin ER, oxycodone CR, glipizide XL, and others are designed to release slowly. After surgery, they often pass through the gut too fast. Up to 47% of these drugs require switching to immediate-release versions.
- Calcium and vitamin D: Absorption drops sharply. Over 70% of patients need higher doses-often 1,500-2,000 mg of calcium citrate daily, split into doses, and taken with food.
- Antidepressants and antiepileptics: Drugs like sertraline, phenytoin, and lamotrigine show variable absorption. Blood levels must be checked regularly.
- Immune suppressants: Tacrolimus and cyclosporine require strict monitoring. A 10% drop in absorption can lead to organ rejection.
Even over-the-counter meds like ibuprofen or aspirin can cause problems. Some patients report stomach irritation after surgery-not because of the drug, but because the pill sits in the small pouch, not dissolving properly.
What to Do: Practical Adjustments
You can’t just keep taking the same pills the same way. Here’s what works:- Switch extended-release to immediate-release. For metformin, use 500mg three times a day instead of 1,000mg ER once a day. For oxycodone, use immediate-release every 4-6 hours as needed. Your pharmacist can help with exact conversions.
- Use liquids or crushable tablets. In the first 3-6 months after surgery, liquid forms are safest. If a pill is not enteric-coated or extended-release, it can be crushed and mixed with water or applesauce. Always check with your pharmacist first.
- Take meds on an empty stomach. Levothyroxine, iron, and some antibiotics work best 30-60 minutes before food. Food can block absorption in the altered gut.
- Take fat-soluble drugs with meals. Vitamin D, cyclosporine, and some antifungals need fat to be absorbed. Take them with a protein-rich meal.
- Split doses. Calcium should be taken in 500-600 mg doses, no more at once. More than that won’t be absorbed.
- Use calcium citrate, not carbonate. Citrate doesn’t need acid to dissolve. Carbonate does-and after surgery, there isn’t enough.
Many patients report their pills ‘not dissolving’-a real issue. A 2020 study found 65% of patients had this complaint. Switching to liquid or crushing non-ER tablets solves this in most cases.
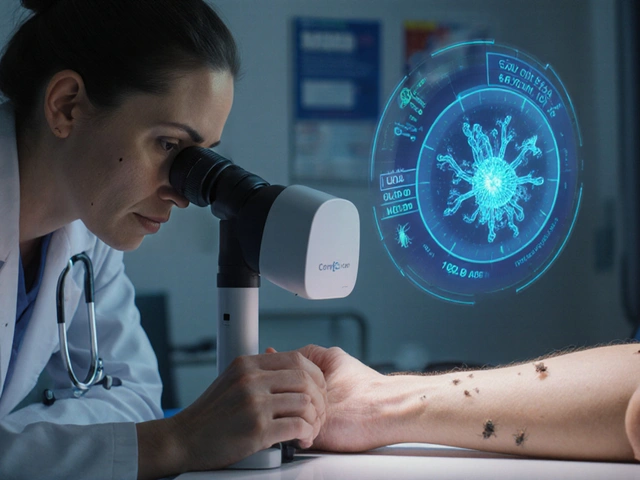
Monitoring Is Non-Negotiable
You can’t guess your way through this. Blood levels matter.The American Society for Metabolic and Bariatric Surgery recommends therapeutic drug monitoring for 12 high-risk medications. That means regular blood tests:
- Warfarin: INR checked weekly for the first month, then monthly
- Levothyroxine: TSH checked at 6 weeks, then every 3 months
- Phenytoin, tacrolimus, cyclosporine: Trough levels checked every 2-4 weeks post-op, then quarterly
- Antidepressants: Levels checked at 3 and 6 months
One patient in Bristol, after sleeve surgery, kept taking her sertraline at 100mg daily. She felt worse, not better. A blood test showed levels were half of what they were before surgery. Her doctor increased it to 150mg, and her mood improved within three weeks.
Without monitoring, you’re flying blind. And that’s dangerous.

Pharmacists Are Your Secret Weapon
Most doctors don’t know the details of post-bariatric pharmacokinetics. Pharmacists do.A 2022 survey found 78% of community pharmacists felt unprepared to handle bariatric patients. But those who’ve had training-40 hours of specialized education, like the program at the University of North Carolina-cut medication errors by over half.
Ask your pharmacist: ‘Is this pill still going to work after my surgery?’ Bring your list of meds to every appointment. Use a tool like the NHS’s 5-step assessment: check the drug, the surgery type, the formulation, the timing, and the patient’s symptoms.
There are now over 200 specialized bariatric pharmacy positions in the U.S., and salaries average $145,000. That’s how critical this field has become.
What’s Changing Now
The field is evolving fast. The FDA now requires new oral drugs to include bariatric surgery data in their labels. In January 2024, the European Medicines Agency made it mandatory.New formulations are on the horizon:
- Subcutaneous implants: ITCA 650, a daily exenatide implant, works just as well after RYGB as it does in non-surgical patients-unlike oral GLP-1 drugs.
- pH-adaptive capsules: Being tested in Copenhagen, these capsules only release their contents when they reach the right pH, even in a high-pH stomach. Early results show 85% absorption vs. 45% for standard pills.
- AI dosing calculators: Used in 83 U.S. hospitals, these tools adjust doses based on surgery type, weight, and drug properties. They’ve cut dosing errors by 41%.
Soon, pharmacogenomics-testing your genes for how you metabolize drugs-may be part of pre-surgery planning. If your body naturally breaks down certain meds faster, your doctor can adjust before you even go under the knife.
Final Takeaway
Bariatric surgery saves lives-but it doesn’t make your body forget how to absorb medicine. If you’re post-op, your meds are not the same. What worked before may not work now. Don’t assume. Don’t wait for symptoms to get worse. Talk to your pharmacist. Get blood tests. Switch formulations if needed. Your health depends on it.Do all bariatric surgeries affect medication absorption the same way?
No. Sleeve gastrectomy mainly reduces stomach size and raises pH, causing mild absorption changes. Roux-en-Y gastric bypass bypasses key parts of the small intestine, leading to major drops in absorption for many drugs. Biliopancreatic diversion causes the most severe changes. Gastric banding has the least impact on absorption.
Can I still take extended-release pills after bariatric surgery?
Usually not. Extended-release pills rely on slow movement through the GI tract to release medication over time. After bypass surgery, drugs move too quickly through the shortened pathway and don’t have enough time to fully dissolve. Most patients need to switch to immediate-release versions. Always check with your pharmacist before making changes.
Why does my thyroid medication not work anymore after gastric bypass?
Levothyroxine is absorbed in the upper small intestine-the same area bypassed in RYGB. Studies show 25-30% less absorption after surgery. Most patients need a 20-50% dose increase. Always get your TSH levels checked 6 weeks after surgery and adjust accordingly.
Should I crush my pills after bariatric surgery?
Only if they’re not extended-release or enteric-coated. Crushing those types can cause dangerous overdoses or reduce effectiveness. For regular tablets, crushing and mixing with water or soft food can help them dissolve better in the smaller stomach. Always confirm with your pharmacist first.
How often should I get blood tests for my medications after surgery?
It depends on the drug. For warfarin, check INR weekly for the first month, then monthly. For thyroid meds, check TSH at 6 weeks, then every 3 months. For drugs like phenytoin or tacrolimus, check trough levels every 2-4 weeks initially, then quarterly. Your care team should provide a schedule.
What’s the best form of calcium to take after bariatric surgery?
Calcium citrate. Unlike calcium carbonate, it doesn’t need stomach acid to dissolve-something you lack after surgery. Take 1,200-2,000 mg per day, split into doses of 500-600 mg, and take with food for best absorption.
Can I take my medications with coffee or tea after surgery?
It’s best to avoid coffee, tea, and other beverages for 30-60 minutes before and after taking meds. Caffeine can interfere with absorption, and tannins in tea bind to iron and some antibiotics. Water is the safest choice.
Why do I have to take so many more pills now?
Because extended-release pills are replaced with multiple immediate-release doses. Instead of one 500mg metformin ER tablet, you might take three 500mg tablets a day. Calcium and vitamin D also need to be split into smaller doses. It’s not more medication-it’s the same total amount, just spread out to match how your body absorbs it now.





Zac Gray
November 19, 2025 AT 01:16Man, I wish I’d known this before I went under the knife. Took my metformin ER like a champ for six months post-sleeve until my A1C shot up to 8.2. Pharmacist caught it-switched me to 500mg three times a day. My glucose’s been stable since. Why do docs assume we all know this stuff? We’re just trying not to die here.
Steve and Charlie Maidment
November 19, 2025 AT 17:31So you’re telling me all these people are just taking pills like normal after surgery? 😂 I bet half of them are just floating on placebo vibes. My cousin had RYGB and still takes his 1000mg metformin ER like it’s a magic bean. He’s on insulin now. Classic.
Michael Petesch
November 20, 2025 AT 17:28It is truly remarkable how the anatomical alterations induced by bariatric procedures fundamentally disrupt the pharmacokinetic profiles of orally administered pharmaceuticals. The reduction in gastric acidity, coupled with the bypassing of the duodenum, significantly impairs dissolution and absorption mechanisms that have been evolutionarily optimized over millennia. This phenomenon, while well-documented in clinical literature, remains grossly undercommunicated to postoperative patients. A systemic educational intervention is not merely advisable-it is imperative.
Ellen Calnan
November 22, 2025 AT 17:21I cried when I found out my levothyroxine wasn’t working. Not because I was tired (though I was-like, ‘can’t-get-off-the-couch’ tired), but because I thought I was failing. Like my body betrayed me. Then I found a bariatric pharmacist who didn’t treat me like a problem to fix. She gave me a new dose, a schedule, and a hug. I’m not just surviving now-I’m living. If you’re post-op and your meds feel like they’re ghosting you? Don’t blame yourself. Blame the anatomy. And then go talk to a pharmacist. They’re the real heroes.
Richard Risemberg
November 23, 2025 AT 14:15Let’s be real-this isn’t just about pills. It’s about reclaiming your life after surgery. You go from being a person who chugs a daily pill to a person who’s got a little pharmacy on the counter: calcium citrate at breakfast, levothyroxine before coffee, immediate-release metformin with lunch, then dinner, then bedtime vitamins. It’s a whole new routine. But guess what? It works. And when your blood work comes back clean? That’s the sweetest high you’ll ever get. No cap.
Andrew Montandon
November 24, 2025 AT 03:14Wait-so crushing pills is okay? But only if they’re NOT extended-release? And not enteric-coated? And you have to check with the pharmacist? Okay, okay, okay. I’m writing this down. Like, actual pen and paper. Also, calcium citrate > carbonate. Got it. And why is no one talking about this in med school? This is life-or-death stuff. 🙏
Sam Reicks
November 24, 2025 AT 03:28fake science alert. they just want you to buy more pills. the body adapts. you dont need to take 3 metformin a day. theyre just pushing pharma profits. also calcium citrate? its just a scam. eat more cheese. and why do they say to take meds on empty stomach? thats when your stomach is most acidic. they dont know what theyre doing. #flatearthmedicine
Chuck Coffer
November 25, 2025 AT 14:26Of course your meds don’t work. You didn’t do the surgery right. If you’d just lost weight the old-fashioned way-no scalpel, no drama-you wouldn’t have this problem. But no, you had to go the ‘easy’ route. Now you’re paying the price. And don’t even get me started on crushing pills. That’s just asking for trouble.
Christopher Robinson
November 25, 2025 AT 14:54Thank you for this. Seriously. I’m 11 months post-RYGB and I just found out my warfarin levels were all over the place because I was still taking it with food. Switched to empty stomach, got my INR checked, now I’m in range. Also, my pharmacist gave me a laminated card with all my med adjustments. I carry it everywhere. 🤝💊
James Ó Nuanáin
November 27, 2025 AT 11:07While I am profoundly impressed by the clinical rigour of this exposition, I must note that the American medical establishment remains woefully underprepared for the nuanced pharmacokinetic implications of bariatric intervention. In the United Kingdom, we have had specialized bariatric pharmacy clinics since 2015. Here, pharmacists are embedded within surgical teams. We do not leave patients to fend for themselves. One wonders whether your reliance on ‘pharmacists’ as a solution is not merely a symptom of a broken healthcare infrastructure.
Nick Lesieur
November 27, 2025 AT 19:58lol at the 145k pharmacist salary. someone’s gotta pay for all these new pills. i’m sure the hospital loves it. my cousin’s on 8 different meds now after sleeve. he’s got a pill organizer that looks like a space shuttle. he’s not healthier-he’s just more expensive.
Angela Gutschwager
November 28, 2025 AT 10:39