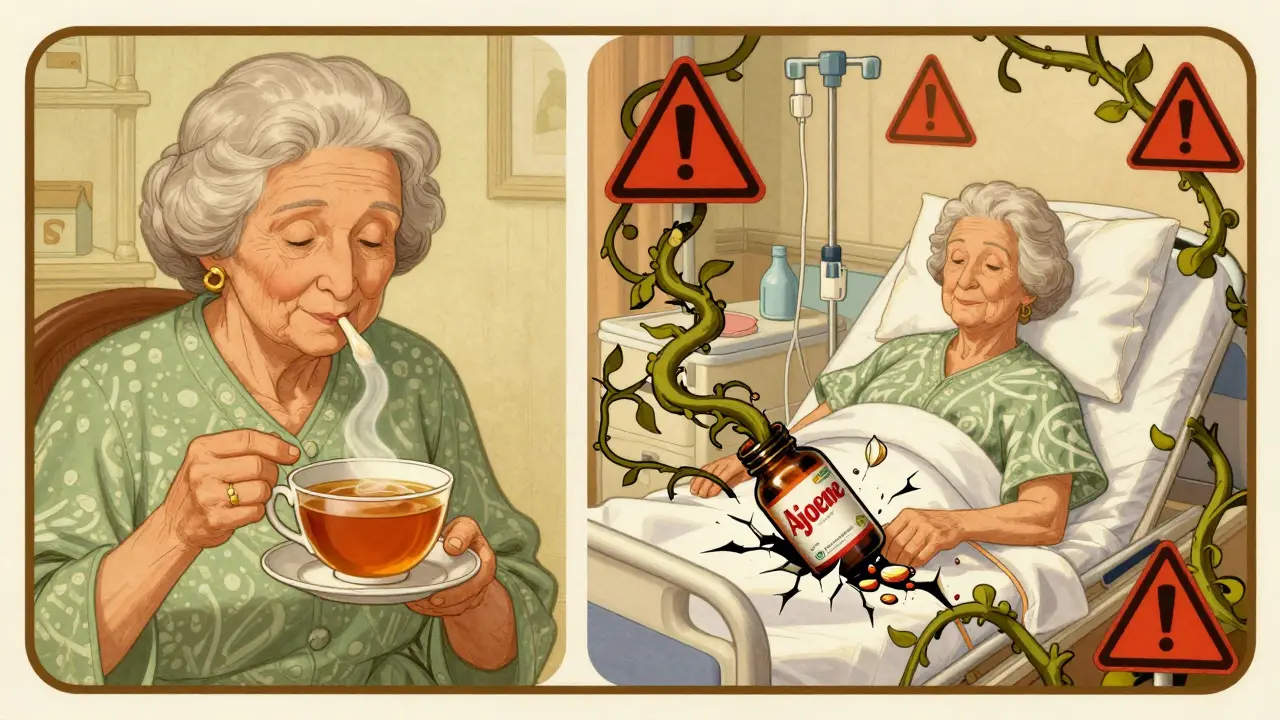
Many people take garlic supplements thinking they’re just boosting heart health or fighting colds. But if you’re on a blood thinner-like warfarin, apixaban, or rivaroxaban-garlic could be quietly putting you at risk for dangerous bleeding. This isn’t theoretical. Real people have ended up in emergency rooms with uncontrolled nosebleeds, internal bleeding after surgery, or even spinal hematomas-all because they didn’t realize garlic supplements act like a mild blood thinner themselves.
How Garlic Interacts with Blood Thinners
Garlic isn’t just a flavor in your pasta sauce. The active compound in garlic supplements, called ajoene, directly interferes with how platelets stick together. Platelets are the tiny cells in your blood that form clots to stop bleeding. When you take an anticoagulant, you’re already slowing down your body’s clotting system. Add garlic on top, and you’re doubling down on that effect.
Studies show garlic can inhibit platelet function by 20-40% at standard supplement doses. That’s similar to low-dose aspirin. But unlike aspirin, which doctors monitor and adjust, garlic supplements are sold without oversight. A 1998 case series in Chest found that people taking warfarin who also used garlic supplements saw their INR levels jump by 1.0 to 2.5 points. INR above 4.0 is considered dangerous-it means your blood takes much longer to clot, increasing the chance of spontaneous bleeding.
The problem isn’t just warfarin. Even newer blood thinners like apixaban and dabigatran can interact with garlic. One Reddit user reported severe nosebleeds lasting over 30 minutes after taking 900 mg of garlic daily with apixaban. That’s not an isolated case. Emergency rooms see these incidents more often than you’d think.
Not All Garlic Supplements Are the Same
Here’s where things get tricky: not all garlic supplements are created equal. The amount of ajoene-the compound that causes the bleeding risk-varies wildly depending on how the supplement is made.
- Oil macerates (garlic soaked in oil) contain the highest levels-up to 1.0 mg of ajoene per gram.
- Standard powdered garlic pills (the most common type) have about 0.1-0.3 mg/g.
- Aged garlic extract (like Kyolic) has almost no ajoene and shows far less antiplatelet activity.
Most supplements you buy at the store are powdered garlic. A typical 600-1,200 mg capsule equals about 5,000-7,000 mg of fresh garlic. That’s a lot. And since the label rarely tells you how much ajoene is in it, you’re guessing your risk.
That’s why some people take garlic supplements for years with no issues-maybe they’re using aged garlic. Others end up bleeding because they’re on a high-potency oil extract and didn’t know the difference.
Who’s at the Highest Risk?
It’s not just anyone on blood thinners. Certain situations make garlic especially dangerous:
- Surgery patients-The American Society of Anesthesiologists says to stop garlic supplements at least 14 days before any surgery. Why? Because during operations, even small amounts of bleeding can become life-threatening. A 2012 study in the Annals of the Royal College of Surgeons found two patients having colon surgery developed uncontrolled oozing from capillaries-both had been taking garlic supplements daily. They needed emergency open surgery and temporary colostomies.
- Dental work-Even a routine tooth extraction can cause prolonged bleeding if you’re on garlic and anticoagulants.
- Neurosurgery or spine procedures-A 2019 case report described an elderly man who developed a spinal hematoma after taking 2,400 mg of garlic daily. He needed emergency surgery to remove the blood clot pressing on his spine.
- Prostate surgery-A 2001 case in Urology documented a patient bleeding for four hours after a prostate procedure because he’d been taking garlic supplements.
And here’s the scary part: 68% of patients in one 2017 study kept taking garlic supplements within seven days of their scheduled surgery-even after being asked about herbal use. Most didn’t think garlic counted as a “supplement.”
How Common Is This Problem?
It’s more common than you think. In 2022, over 3.1 million Americans over 65 were taking both garlic supplements and anticoagulants. That’s based on data from the National Health Interview Survey. Globally, garlic supplement sales hit $1.27 billion in 2022-and they’re growing fast.
But awareness? Almost nonexistent. A 2022 GoodRx survey found that 83% of garlic supplement users had no idea it could interact with blood thinners. Two-thirds never told their doctor about taking it.
And it’s not just older adults. Younger people are popping garlic pills for “heart health” or “immune support,” thinking it’s harmless. But if you’re on a blood thinner, “harmless” doesn’t apply.
What Experts Say
Medical organizations are united on this:
- The American Heart Association says garlic supplements should be used with “extreme caution” if you’re on anticoagulants.
- The American Society of Anesthesiologists lists garlic as a “high-risk herbal product” that must be stopped before surgery.
- The European Medicines Agency now requires garlic supplements to carry warnings about anticoagulant interactions.
Dr. Pieter Cohen from Harvard puts it bluntly: “Garlic supplements can increase the levels and effects of some medications for heart health, such as blood thinners-causing bleeding.”
Some studies try to downplay the risk. A 2018 meta-analysis in Nutrients found only small INR increases. But those studies didn’t account for high-potency supplements or surgical contexts. The real-world evidence-emergency room visits, surgical complications, case reports-tells a different story.

What Should You Do?
If you’re on a blood thinner:
- Stop taking garlic supplements-at least 7 to 14 days before any surgery, dental work, or invasive procedure.
- Ask your doctor or pharmacist-Don’t assume they know. Say: “I take garlic pills. Is that safe with my blood thinner?”
- Check your supplement label-If it says “aged garlic extract,” it’s lower risk. If it says “garlic oil” or “standardized to allicin,” it’s higher risk.
- Don’t switch to another herb-Ginkgo, fish oil, and ginseng also interact with blood thinners. Just because it’s “natural” doesn’t mean it’s safe.
- Track your INR-If you’re on warfarin, your doctor should check your INR more often if you’re using garlic.
And if you’re not on a blood thinner but take garlic supplements, still talk to your doctor before surgery. Many people don’t realize they’re on blood thinners until they start bleeding.
The Bigger Picture
The supplement industry doesn’t have to prove safety before selling. The FDA doesn’t test garlic pills for potency or consistency. A 2019 FDA warning found that garlic supplements varied by up to 15-fold in active ingredient levels between brands. One bottle might be harmless. Another could be a hidden danger.
Only 42% of manufacturers follow FDA labeling guidelines. And only 37% even link to the NIH’s LiverTox database, which tracks drug-supplement interactions.
There’s hope on the horizon. The FDA is working on new labeling rules requiring ajoene content to be listed-expected by mid-2024. Some companies, like Kyolic, are already making “ajoene-free” aged garlic extracts. But until then, assume every garlic supplement has enough ajoene to matter.
Garlic in food? Fine. A clove or two in your cooking won’t hurt. But pills? Powders? Oils? Those are concentrated, unregulated, and potentially dangerous when combined with blood thinners.
It’s not about fear. It’s about awareness. You wouldn’t mix alcohol with your medication. Don’t treat garlic supplements like harmless candy.
Can I take garlic supplements if I’m on warfarin?
It’s not recommended. Garlic can increase your INR levels by 1.0 to 2.5 points, pushing you into a dangerous range where bleeding risk rises sharply. Even if your INR is stable now, garlic can cause sudden spikes. Most doctors advise stopping garlic supplements at least 7-14 days before any surgery or procedure. If you’re on warfarin, talk to your provider before taking any garlic product.
Is aged garlic extract safer than regular garlic supplements?
Yes, aged garlic extract is significantly safer. The aging process breaks down ajoene, the compound responsible for antiplatelet effects. Studies show aged garlic extract has up to 98% less antiplatelet activity than raw garlic or oil-based supplements. Brands like Kyolic are specifically marketed as low-risk for people on blood thinners. But even then, it’s best to check with your doctor before starting.
How long does garlic stay in your system?
Garlic’s antiplatelet effects can last up to 72 hours after taking a dose. But because it irreversibly blocks platelet function, your body needs to make new platelets to recover fully. That takes about 7-10 days. That’s why doctors recommend stopping garlic supplements at least 7-14 days before surgery. Even if you stop today, the effect won’t disappear overnight.
What are the signs of bleeding from garlic and blood thinners?
Watch for: prolonged nosebleeds (over 20 minutes), unusual bruising without injury, blood in urine or stool, excessive bleeding from cuts, headaches or dizziness (possible brain bleed), or sudden back pain (possible spinal bleed). If you’re on a blood thinner and notice any of these after starting garlic, stop the supplement and seek medical help immediately.
Do all garlic supplements have the same effect?
No. Garlic oil macerates and powdered garlic pills have the highest levels of ajoene and pose the greatest risk. Aged garlic extract has very little ajoene and is much safer. But most labels don’t tell you which type you’re getting. If it says “standardized to allicin” or “enteric-coated garlic powder,” it’s likely high-risk. Look for “aged garlic extract” if you must use garlic and are on anticoagulants.
Should I stop garlic supplements before a colonoscopy or dental cleaning?
Yes. Even minor procedures can cause bleeding if your blood can’t clot properly. Colonoscopies involve biopsies or polyp removal. Dental cleanings can cause gum bleeding. Both are low-risk in healthy people-but dangerous if you’re on blood thinners and garlic. Stop garlic supplements at least 7 days before any procedure, even if it’s not surgery. Always tell your provider you’re taking them.




Janette Martens
December 29, 2025 AT 18:58so i took garlic pills for my cold last winter and my nose was bleeding like a faucet for 3 days… i thought i was just sick but turns out i was on apixaban and didnt know garlic was a hidden bomb. my dr was pissed i didnt tell her. dumbass move. learn from my mess.
Marie-Pierre Gonzalez
December 29, 2025 AT 21:22Thank you for this extremely well-researched and vital post. As a registered nurse in Ontario, I’ve seen too many patients present with unexplained bruising and prolonged bleeding after minor procedures-all because they believed ‘natural’ meant ‘safe.’ I now routinely ask about herbal supplements during intake, and I make sure to emphasize that garlic supplements are not ‘just garlic.’ The lack of regulation in this industry is alarming. Please, everyone: speak up, ask questions, and protect yourself.
Louis Paré
December 30, 2025 AT 23:48Let’s be real-this is just another example of the medical-industrial complex trying to scare people out of natural remedies so they keep buying prescription drugs. Garlic’s been used for millennia. You think a few lab rats in a 1998 case series are more credible than centuries of folk medicine? The real danger is blind trust in pharmaceuticals and their fearmongering partners. Also, INR fluctuations happen all the time. Chill out.
Ellen-Cathryn Nash
January 1, 2026 AT 17:21Wow. Just… wow. I’ve been popping garlic capsules like candy for years because my yoga instructor said it ‘cleanses the blood.’ I’m on rivaroxaban. I just threw out my entire bottle. I feel like a naive idiot. But honestly? I’m grateful. This could’ve killed me. I’m telling everyone I know. This isn’t fear-it’s responsibility.
James Hilton
January 3, 2026 AT 10:45Garlic pills = nature’s aspirin, but without the FDA’s ‘warning label’ sticker. You wouldn’t chug whiskey before surgery, so why chug garlic oil? 😅
Mimi Bos
January 3, 2026 AT 12:48i had a tooth pulled last year and it bled for 2 hours. i thought it was just bad luck… then i remembered i’d been taking garlic pills for my ‘immune boost.’ my dentist was like ‘did you tell anyone you were taking that?’ nope. my bad. lesson learned. always ask.
Kelsey Youmans
January 3, 2026 AT 18:26Thank you for sharing this critical information with such clarity and depth. As someone who manages anticoagulation therapy for elderly patients, I can attest that the majority are unaware of herb-drug interactions. The supplement industry operates in a regulatory gray zone that puts vulnerable populations at risk. We need mandatory labeling, provider education, and public awareness campaigns-not just anecdotal Reddit posts. This is a public health issue.
Sydney Lee
January 4, 2026 AT 02:21Let’s not romanticize ignorance. The fact that 83% of users are unaware of this interaction isn’t a failure of education-it’s a failure of capitalism. Companies profit from selling unregulated, untested, and potentially lethal products under the guise of ‘wellness.’ Ajoene isn’t some mystical herb-it’s a pharmacologically active compound, and its absence from labeling is a crime. The FDA’s delay in enforcing disclosure isn’t negligence-it’s complicity. Until labels state ajoene content in milligrams, this will keep happening. And when it does, don’t blame the patient. Blame the billion-dollar industry that sold them poison as a ‘health boost.’