Frailty & Medication Risk Calculator
How This Works
Based on clinical guidelines for frail older adults, this tool estimates your risk of medication side effects using:
- Number of medications you take daily
- Your frailty status (based on 5 clinical criteria)
Medication Count
Frailty Assessment
Check all that apply (based on clinical criteria):
Your Risk Assessment
Important: This tool is for informational purposes only. Always consult your healthcare provider before making medication changes.
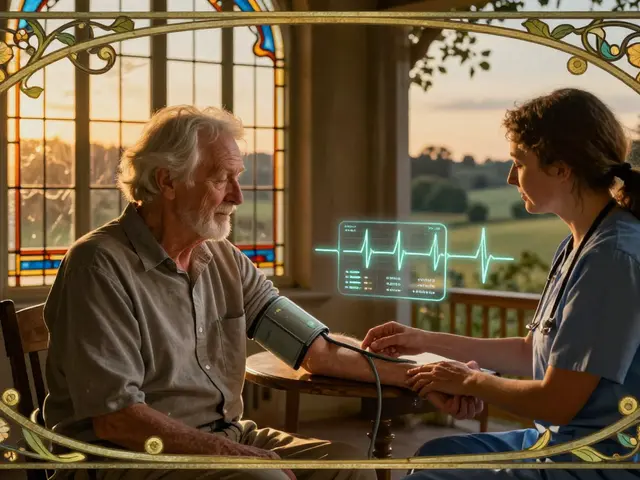
More than half of older adults in the U.S. are taking five or more medications every day. For someone who’s frail-someone who’s lost strength, moves slowly, gets tired easily-each pill adds risk. Not all of them are helping. Some are making things worse. Dizziness. Falls. Confusion. Constipation. These aren’t just side effects. They’re warning signs that the medication list has grown too big, too messy, and too dangerous.
What Frailty Really Means
Frailty isn’t just being old. It’s a measurable condition. The medical definition looks at five things: unintentional weight loss, feeling exhausted most days, weak grip strength, walking slower than usual, and low physical activity. If you have three or more of these, you’re frail. Two? You’re pre-frail. Zero? You’re robust. This isn’t guesswork. It’s based on real, tested criteria used in clinics and research.
Frailty doesn’t happen overnight. It builds slowly. But once it’s there, it makes the body less able to handle stress-like a new medication. A drug that might be fine for a healthy 70-year-old can knock a frail 85-year-old off balance. That’s why the number of pills matters more than just whether someone meets the technical definition of polypharmacy.
Polypharmacy Isn’t Just Many Pills-It’s the Wrong Pills
Polypharmacy means five or more daily medications. Hyper-polypharmacy? Ten or more. But the real problem isn’t the count. It’s the overlap, the duplication, the outdated prescriptions. Someone might be on a blood pressure pill that causes dizziness, a painkiller that causes constipation, and a sleep aid that makes them confused. All three were prescribed for a real reason. But together? They create a perfect storm.
Studies show that for every extra medication an older adult takes, their chance of becoming frail increases by 12%. That’s not a small risk. And it works both ways: frail people are more likely to be prescribed more drugs because they have more conditions. But those drugs then make them even frailer. It’s a cycle.
And the numbers are climbing. In 1999, about 23% of older adults took five or more meds. By 2018, it was over 44%. Among those with heart disease? More than 60%. Women, white individuals, and those with less education are more likely to be affected. But the highest rates? In hospitals-over 96% of hospitalized older adults are on polypharmacy. That’s not because they need it. It’s because care is fragmented. Each specialist adds a drug. No one steps back to see the whole picture.
The Real Cost: Falls, Hospitalizations, and Lost Independence
Medication side effects in frail older adults don’t just cause discomfort. They cause crises. Dizziness leads to falls. Falls lead to broken hips. Broken hips lead to hospital stays. Hospital stays lead to delirium. Delirium leads to long-term decline.
One study of nursing home residents found that 78% of those on eight or more medications had at least one adverse drug event every month. The top three? Dizziness, falls, and constipation. Constipation alone can lead to bowel obstructions, emergency visits, and even death if ignored.
And it’s expensive. Medication-related problems cost the U.S. healthcare system $30 billion a year. Around 125,000 to 300,000 preventable deaths happen annually because of these issues. That’s not just a statistic. That’s a grandmother who fell and never walked again. A grandfather who stopped eating because his stomach hurt from his pills. A mother who couldn’t live alone anymore because she forgot which pill to take when.
Deprescribing: Taking Pills Away on Purpose
Most people assume more drugs mean better care. But sometimes, less is more. Deprescribing isn’t stopping meds randomly. It’s a careful, step-by-step process of removing drugs that no longer help-or that hurt more than they help.
Tools like the Beers Criteria and START/STOPP guidelines help doctors spot inappropriate medications. The Beers Criteria list drugs that are risky for older adults-like benzodiazepines for sleep or anticholinergics for overactive bladder. These drugs can cause confusion, memory loss, and falls. STOPP tells providers when they’re missing a needed drug, like a bone-strengthening medication for someone with osteoporosis.
When these tools are used properly, inappropriate prescribing drops by 30% to 50%. But they only work if someone takes the time to use them. Most primary care doctors say they rarely review medication lists for deprescribing because they’re rushed. That’s why pharmacist-led programs are making a difference.
One successful method is the 3-Step Method developed by Dr. Cynthia Boyd at Johns Hopkins:
- Review the full medication list-prescription, over-the-counter, supplements.
- Talk with the patient: What matters to you? Are you having side effects? Do you feel better or worse since starting this?
- Monitor after stopping: Watch for changes in energy, balance, digestion, mood.
This approach reduces inappropriate medications by 28% in six months. And 92% of patients stick with it because they’re part of the decision.
What Works in Real Life
Not all solutions are high-tech. Sometimes, the simplest changes make the biggest difference.
- Pharmacist-led medication therapy management reduces adverse events by 34%. Pharmacists review all meds, check for interactions, and call doctors to suggest changes.
- Comprehensive geriatric assessment clinics bring together doctors, nurses, pharmacists, and social workers. In 12 months, they cut polypharmacy by 22%.
- Medication Check-Up programs teach patients how to read their pill bottles, use pill organizers, and recognize warning signs. Participants improved their understanding by 47%.
Technology is helping too. In January 2024, the FDA approved the first AI-powered deprescribing tool: MedWise Risk Score. It analyzes a patient’s full medication list and predicts the risk of side effects. In trials, it cut adverse events by 37%.
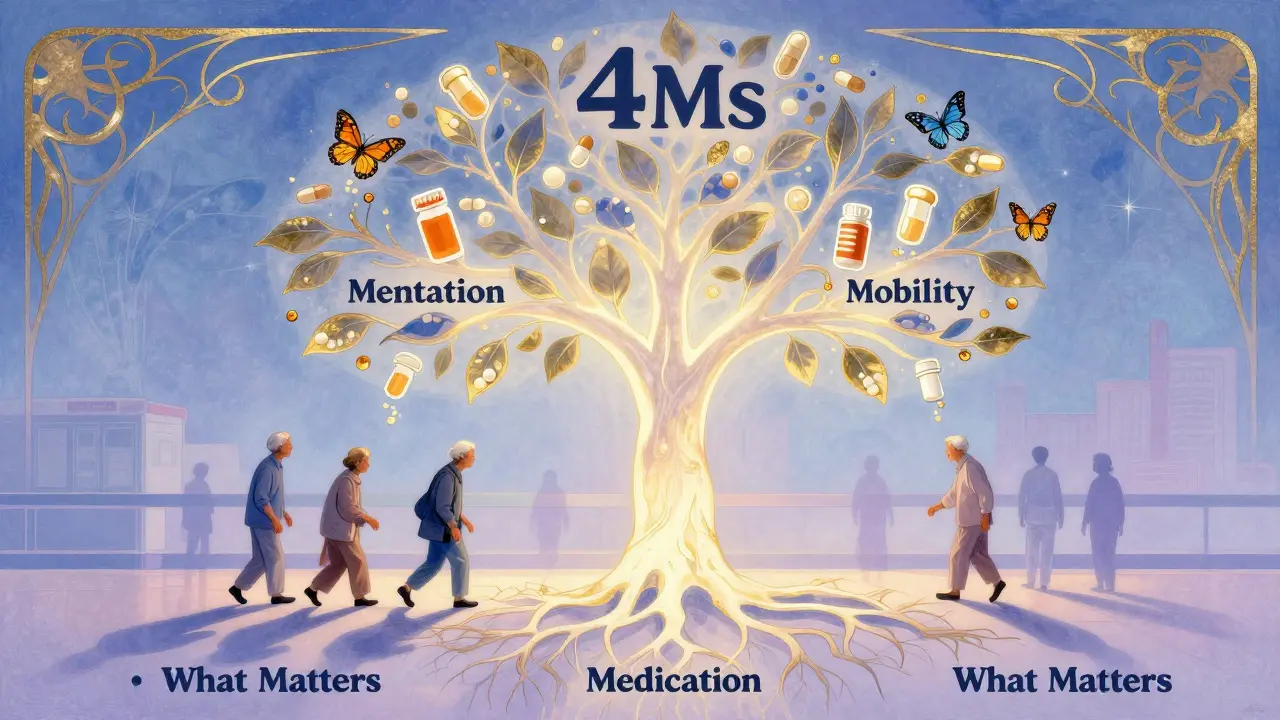
The American Geriatrics Society’s Age-Friendly Health Systems initiative now includes over 2,850 hospitals and clinics. They use the 4Ms Framework: What Matters to the patient, Medication (are they appropriate?), Mentation (is there confusion or depression?), and Mobility (can they move safely?). When all four are addressed, inappropriate polypharmacy drops by 24%.
Why It’s So Hard to Change
Even when the evidence is clear, change is slow. Why?
- Fragmented care: A cardiologist prescribes one drug, a neurologist another, a pain specialist a third. No one sees the whole list.
- Lack of EHR alerts: Only 38% of U.S. hospitals have electronic systems that flag potentially harmful combinations.
- Patient fear: Over half of older adults worry that stopping a pill will make them sicker. Many think their meds are keeping them alive-even when they’re not.
- Time: A proper medication review takes 15 to 20 minutes. Most primary care visits are 10.
And then there’s the culture. Doctors are trained to add treatments. Not to take them away. But in frail older adults, the goal isn’t to treat every condition. It’s to preserve quality of life.
What You Can Do
If you or a loved one is on five or more medications:
- Ask: “Which of these are still helping me? Which might be causing problems?”
- Bring a complete list-every pill, vitamin, and supplement-to every appointment.
- Ask the pharmacist to do a free medication review. Most offer it.
- Watch for new symptoms: dizziness, confusion, constipation, fatigue. These aren’t normal aging. They’re red flags.
- Don’t stop a pill on your own. But do ask for a plan to safely reduce or remove one.
One study found that 76% of people who participated in a deprescribing trial successfully stopped at least one medication-without harm. And 32% reported better quality of life. That’s not a miracle. That’s common sense.
The Future Is Clearer, Not Heavier
The goal isn’t to eliminate all medications. It’s to make sure every pill has a purpose. For frail older adults, the best treatment isn’t another drug. It’s removing the ones that are doing more harm than good.
By 2030, the WHO aims to cut severe medication-related harm by 50%. The NIH is funding a $15 million trial to test a pharmacist-led intervention for frail older adults. AI tools are getting smarter. More hospitals are adopting the 4Ms Framework.
But progress depends on people speaking up. On families asking questions. On doctors listening. On systems making time for what matters most: not just living longer, but living well.
What’s the difference between polypharmacy and appropriate medication use?
Polypharmacy simply means taking five or more medications daily. But not all polypharmacy is inappropriate. Someone with heart failure, diabetes, and arthritis may need several drugs to stay healthy. The problem isn’t the number-it’s whether each medication is still necessary, effective, and safe for that person. Appropriate use means every drug has a clear purpose, is monitored for side effects, and aligns with the patient’s goals-like staying independent or avoiding falls.
Can stopping a medication make someone sicker?
Sometimes, yes-but only if it’s done suddenly or without a plan. Medications like blood pressure pills or antidepressants shouldn’t be stopped cold turkey. But many older adults are on drugs that were prescribed years ago and no longer serve a purpose-like a cholesterol pill for someone with advanced dementia, or a sleep aid that causes daytime confusion. When deprescribing is done slowly, with monitoring, the risk of harm is low. In fact, studies show most people feel better after removing unnecessary meds.
Why do doctors keep prescribing more pills instead of cutting back?
Many doctors are trained to treat each condition separately, not the whole person. They’re also under time pressure-most visits are 10 minutes or less. Reviewing a full medication list can take 15 to 20 minutes. Plus, there’s fear: doctors worry about being blamed if a patient gets worse after stopping a drug. But research shows that when deprescribing is done properly-with patient input and follow-up-it’s safe and often improves outcomes.
Are over-the-counter drugs and supplements part of the problem?
Absolutely. Many older adults take daily supplements like melatonin, magnesium, or herbal remedies without telling their doctor. These can interact with prescription drugs. For example, St. John’s Wort can reduce the effectiveness of blood thinners. Calcium supplements can interfere with thyroid meds. Even common painkillers like ibuprofen can raise blood pressure or cause stomach bleeding in frail people. Every pill counts-prescription or not.
How can I help a frail loved one manage their medications?
Start by making a complete list of everything they take-name, dose, frequency, reason. Use a pill organizer and set phone reminders. Go with them to appointments and ask the doctor: “Is this still needed?” “Are there side effects we should watch for?” “Can we try stopping one?” Encourage them to speak up about how they feel. Many older adults don’t want to complain. But if they’re dizzy, tired, or constipated, it’s not normal. It’s a signal.
Reducing side effects from multiple medications isn’t about cutting corners. It’s about choosing what matters. For frail older adults, the best medicine isn’t always another pill. Sometimes, it’s the courage to let go of the ones that are weighing them down.






Renee Stringer
January 21, 2026 AT 02:30It’s not just about the pills-it’s about the system that keeps pushing them. I’ve seen my mother on 12 medications, none of which were reviewed in a year. The doctor barely looked at the list. She’s dizzy all the time, but no one wants to take anything away. It’s easier to prescribe than to think.
And don’t get me started on supplements. That ‘natural’ turmeric capsule? Interacts with her blood thinner. She didn’t even tell her doctor because she thought it was ‘harmless.’
We’re treating symptoms like puzzles to solve, not people to care for. And the cost? Not just financial-it’s dignity.
Crystal August
January 23, 2026 AT 01:12Every single one of these ‘solutions’ is just another bureaucratic band-aid. Pharmacist reviews? Geriatric clinics? AI tools? Please. The real problem is that medicine stopped being about healing and became a revenue stream. Hospitals profit from prescriptions. Pharma funds research. Doctors get bonuses for hitting ‘quality metrics’-which means more prescriptions, not fewer.
Deprescribing sounds nice on paper. In practice? It’s a liability nightmare. Who’s going to take the blame when Grandma gets ‘worse’ after they take away her ‘heart pill’ that was prescribed in 2008?
It’s not broken. It’s designed this way.
pragya mishra
January 23, 2026 AT 23:46Why are we even surprised? In India, we see this too-grandparents on 8+ meds because every specialist adds one. No one talks to each other. The cardiologist doesn’t know the neurologist prescribed a sedative. The pharmacist is too busy counting pills to ask why.
But here’s the truth: we don’t ask because we’re scared. Scared to say ‘no’ to the doctor. Scared that if we stop one pill, something will kill us. But we never ask: what’s killing us right now?
Stop calling it ‘polypharmacy.’ Call it medical neglect.
sagar sanadi
January 25, 2026 AT 17:00AI-powered deprescribing tool? LOL. Next they’ll sell us a robot that tells grandma she’s too old to be alive.
And don’t tell me ‘the 4Ms Framework’ is the answer. That’s just corporate jargon for ‘we’re too lazy to listen.’
Meanwhile, the FDA approves another drug that causes dizziness, then another tool to fix the dizziness. It’s a pyramid scheme with pills.
They don’t want fewer meds. They want more data. More billing codes. More profit.
And you’re all drinking the Kool-Aid.
;-)
clifford hoang
January 25, 2026 AT 20:03Think about it. The entire medical-industrial complex is built on the illusion that more intervention = better outcomes. But what if the real cure is silence? What if the body doesn’t need more chemicals-it needs less noise?
Every pill is a signal. A signal that we’ve outsourced our biology to a system that profits from dysfunction.
Deprescribing isn’t medicine. It’s rebellion. It’s saying: ‘I am not a database of symptoms. I am a human being who deserves to feel my own life.’
And the fact that we need an AI tool to tell us this? That’s the real tragedy.
🫠💊🤯
Arlene Mathison
January 27, 2026 AT 00:45THIS. THIS IS SO IMPORTANT. I helped my dad cut down from 11 to 5 meds last year. He went from barely walking to gardening again. He cried when he said, ‘I feel like myself.’
Don’t wait for a ‘program’ or an ‘AI tool.’ Start today. Write down every pill. Call the pharmacist. Ask the doctor: ‘What happens if we stop this?’
You don’t need permission to care. Just courage.
And if you’re scared? You’re not alone. I was too. But watching him eat breakfast without dizziness? Worth every scary conversation.
Carolyn Rose Meszaros
January 27, 2026 AT 13:44My aunt was on 14 meds. We started with one: the sleeping pill. She hadn’t slept through the night in 3 years. After stopping it? She slept 7 hours. No rebound insomnia. No crashes. Just… rest.
She said, ‘I didn’t realize I was so tired because I was always dizzy.’
It’s not magic. It’s just… not poisoning yourself with 14 different chemicals.
❤️
Greg Robertson
January 28, 2026 AT 17:24I work in a clinic and I see this every day. Doctors want to help, but they’re stretched so thin. I’ve seen a 78-year-old come in for a flu shot and leave with three new scripts-none of which were discussed.
It’s not malice. It’s exhaustion.
But here’s what works: when families show up with a printed list and say, ‘Can we just look at this together?’-that’s when change happens.
Be the person who asks. Even if it’s awkward. Even if it’s 10 minutes before closing.
It matters.
Edith Brederode
January 29, 2026 AT 18:13I just started helping my neighbor, 84, with her meds. She was taking three different antacids, a muscle relaxer, and a sleep aid-all because she had ‘digestive issues’ from the blood pressure pill.
We called her pharmacist. They said, ‘Oh, we flagged that last year. No one followed up.’
So we took the BP pill down by half. Two weeks later, she said, ‘I don’t feel like I’m swallowing rocks anymore.’
It’s not complicated. It’s just… overlooked.
Thank you for writing this. I’m sharing it with everyone.
❤️
Emily Leigh
January 31, 2026 AT 15:03