Sleep Quality Assessment Tool
Sleep Quality Assessment
Answer these questions to get an assessment of your sleep quality. This tool is for informational purposes only and not a substitute for professional medical advice.
Your Sleep Quality Assessment
Ever wonder why a night of tossing and turning can leave you feeling like a zombie? When sleep goes haywire, it’s not just about feeling cranky - the whole body and brain start to malfunction. This article breaks down the science behind sleep disorders, shows what happens inside you when they strike, and gives practical steps to get back on track.
Quick Takeaways
- Sleep is a regulated, brain‑driven process that restores memory, metabolism, and immunity.
- Disorders such as insomnia, sleep apnea, and narcolepsy disrupt specific sleep stages, leading to short‑term fatigue and long‑term health risks.
- Accurate diagnosis often requires a sleep study and a review of lifestyle factors.
- Effective treatments range from behavioral therapy to CPAP machines and medication, depending on the condition.
- Simple habits - consistent schedule, screen curfew, and a cool dark room - can improve most sleep issues.
What Sleep Actually Is
Sleep is not a passive state; it’s an active, highly organized sequence of stages. During a typical night you cycle through non‑rapid eye movement (NREM) stages 1‑3 and rapid eye movement (REM) sleep about four to five times. NREM deep sleep (stage 3) is where the body repairs tissue, releases growth hormone, and consolidates factual memories. REM sleep fuels emotional processing and creativity, and it’s when most vivid dreaming occurs.
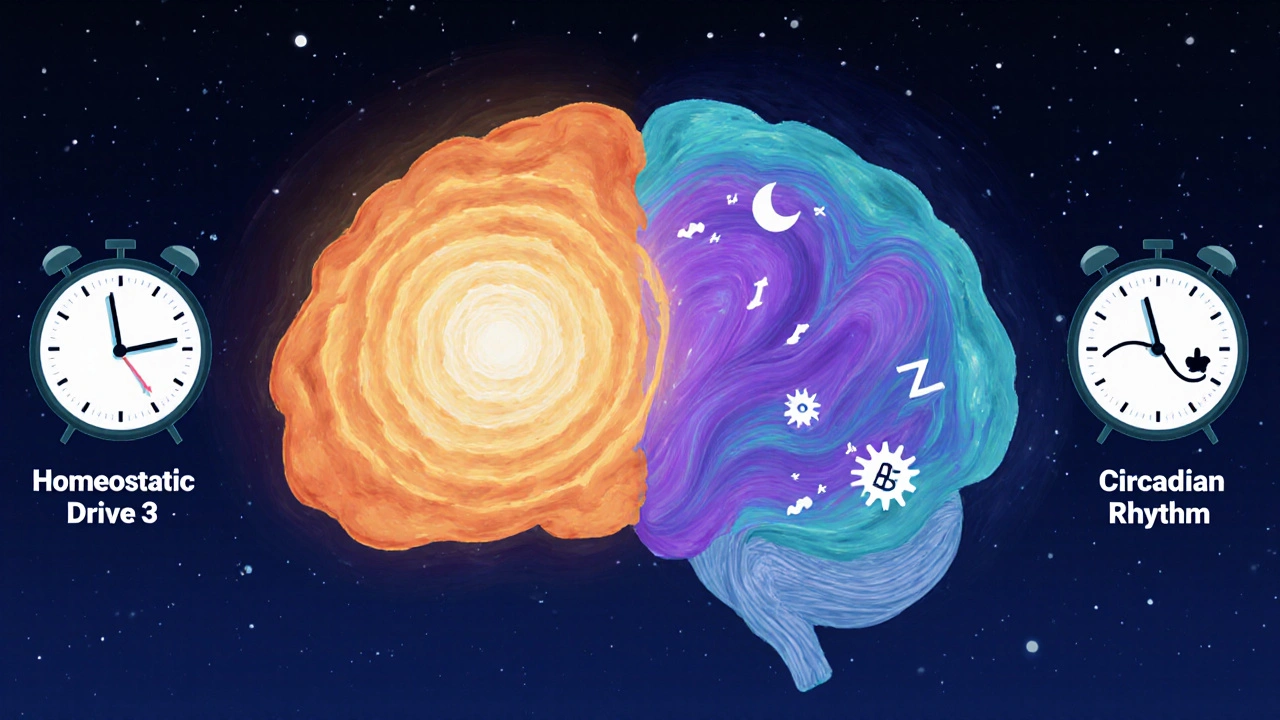
Two master clocks keep this rhythm ticking:
- Homeostatic drive - the longer you stay awake, the stronger the pressure to sleep.
- Circadian rhythm - a 24‑hour internal clock centered in the suprachiasmatic nucleus that tells your body when to feel alert or sleepy.
When either of these systems is out of sync, you’re vulnerable to a sleep disorder.
Introducing the Main Players
Below are the most common sleep disorders. Each definition appears once with Sleep Disorders are medical conditions that disrupt normal sleep patterns, leading to impaired daytime functioning and increased health risks. The following entities are also marked up for knowledge‑graph relevance.
- Insomnia is difficulty falling asleep, staying asleep, or waking up too early, affecting roughly 10% of adults chronically
- Sleep Apnea is a breathing‑related disorder where airway collapse causes repeated pauses in breathing, present in about 22 million Americans
- Narcolepsy is a neurological condition characterized by sudden sleep attacks and cataplexy, affecting 1 in 2,000 people
- Restless Legs Syndrome (RLS) causes an irresistible urge to move the legs, especially at night, impacting 7-10% of the population
- Circadian Rhythm Disorder includes shift‑work disorder and jet lag, where the internal clock is misaligned with the external environment
- REM Sleep Behavior Disorder involves acting out vivid dreams due to loss of muscle atonia during REM sleep
How Each Disorder Disrupts the Body
Understanding the physiological cascade helps you see why a sleepless night feels like a mini‑crash. Below is a snapshot of the most important effects.
- Insomnia - Increases cortisol, spikes blood pressure, and impairs the hippocampus’s ability to store new memories.
- Sleep Apnea - Causes intermittent hypoxia, leading to inflammation, insulin resistance, and a 2‑3‑fold rise in cardiovascular disease risk.
- Narcolepsy - Low levels of hypocretin (orexin) drive sudden REM intrusions, resulting in fragmented sleep architecture and daytime microsleeps.
- RLS - Dopaminergic dysfunction triggers leg movements that fragment NREM sleep, worsening mood and fatigue.
- Circadian Rhythm Disorder - Misaligned melatonin release disrupts hormone balance, causing metabolic slowdown and higher obesity odds.
- REM Sleep Behavior Disorder - Increases risk of neurodegenerative diseases such as Parkinson’s because REM atonia loss may reflect early brainstem pathology.
Diagnosing Sleep Disorders
Because symptoms often overlap, a systematic approach is essential:
- Sleep History - A detailed questionnaire covering bedtime routine, daytime sleepiness, and partner observations.
- Polysomnography (PSG) - An overnight lab test that records brain waves, oxygen levels, heart rate, and muscle activity.
- Home Sleep Apnea Test (HSAT) - A simplified version for suspected obstructive sleep apnea, using a few sensors.
- Multiple Sleep Latency Test (MSLT) - Measures how quickly a person falls asleep in a quiet environment, key for narcolepsy.
Doctors also rule out medical or psychiatric conditions that mimic sleep problems, such as thyroid disorders or depression.

Treatment Options by Disorder
What works best depends on the root cause. Below is a concise guide.
| Disorder | Key Symptoms | Primary Treatment | Long‑Term Risks |
|---|---|---|---|
| Insomnia | Difficulty falling/maintaining sleep | Cognitive‑behavioral therapy for insomnia (CBT‑I), sleep hygiene | Depression, hypertension |
| Sleep Apnea | Loud snoring, witnessed pauses, daytime sleepiness | CPAP therapy, oral appliances, weight loss | Heart disease, stroke, type 2 diabetes |
| Narcolepsy | Sudden sleep attacks, cataplexy, hallucinations | Stimulants (modafinil), sodium oxybate, scheduled naps | Reduced quality of life, injury risk |
| RLS | Urge to move legs, worsening at night | Iron supplements, dopamine agonists, leg stretches | Chronic insomnia, mood disturbances |
| Circadian Rhythm Disorder | Sleep at odd hours, excessive daytime sleepiness | Light therapy, melatonin, scheduled sleep‑wake times | Metabolic syndrome, impaired cognition |
In many cases, a combination of lifestyle tweaks and medical therapy yields the best results.
Everyday Habits to Boost Sleep Health
- Stick to a schedule - Go to bed and wake up within 30 minutes even on weekends.
- Dim the lights 1‑hour before bed - Reduces blue‑light suppression of melatonin.
- Reserve the bedroom for sleep - No work laptops or stressful TV shows.
- Keep the room cool (60‑67°F / 15‑19°C) - Supports the drop in core body temperature needed for sleep onset.
- Limit caffeine after noon - Its half‑life can keep you wired for up to 6hours.
- Exercise regularly, but not right before bedtime - Helps deepen NREM sleep.
- Consider a short (20‑minute) power nap if you’re sleep‑deprived, but avoid late‑day naps that shift your circadian rhythm.
These habits don’t replace professional care but can dramatically reduce the severity of many disorders.
Frequently Asked Questions
Can occasional sleeplessness turn into a chronic disorder?
Yes. A few bad nights are normal, but if you find it hard to fall asleep or stay asleep more than three nights a week for over a month, you may be developing insomnia. Early intervention with CBT‑I often prevents chronic patterns.
Is snoring always a sign of sleep apnea?
Snoring is common, but loud, irregular snoring with observed pauses in breathing strongly suggests obstructive sleep apnea. A home sleep test can confirm the diagnosis.
Do I need a prescription for a CPAP machine?
Yes. A sleep physician must diagnose sleep apnea and prescribe the appropriate pressure settings. Insurance coverage usually requires a documented prescription.
Can diet affect my sleep disorder?
Absolutely. High‑sugar meals can trigger insulin spikes that disturb REM sleep, while magnesium‑rich foods (nuts, leafy greens) support relaxation and improve insomnia symptoms.
Is it safe to use over‑the‑counter sleep aids long‑term?
Most OTC antihistamine‑based pills work for a few nights but can cause tolerance, daytime drowsiness, and anticholinergic side effects. For chronic issues, talk to a doctor about CBT‑I or prescription options.
Got more questions? A sleep specialist can tailor a plan that fits your unique pattern.





Aman Vaid
October 14, 2025 AT 12:28When looking at the mechanisms behind sleep disorders, the interplay between the homeostatic drive and the circadian clock emerges as the central axis of regulation. Prolonged wakefulness elevates adenosine concentrations, which in turn intensify the pressure to fall asleep. If the suprachiasmatic nucleus receives conflicting light cues, melatonin secretion can become mistimed, leading to fragmented sleep architecture. In insomnia, the hyperarousal state sustains elevated cortisol, impairing the consolidation of declarative memory during stage‑3 NREM. Obstructive sleep apnea introduces intermittent hypoxia; each apnea episode triggers sympathetic surges that accelerate atherosclerotic processes. The hypoxic burden also disrupts REM latency, shortening the period in which emotional memory processing occurs. Narcolepsy, on the other hand, is characterized by a deficiency of hypocretin, which destabilizes the boundary between wakefulness and REM sleep. This results in sudden sleep attacks and cataplexy, often misinterpreted as ordinary fatigue. Restless Legs Syndrome reflects dopaminergic dysregulation, causing periodic limb movements that fragment non‑REM sleep stages. Circadian rhythm disorders, such as shift‑work disorder, misalign peripheral clocks, thereby impairing glucose tolerance and increasing obesity risk. REM Sleep Behavior Disorder removes the atonia normally present in REM, allowing dream enactment that can cause injury. Long‑term untreated sleep apnea has been linked to insulin resistance, hypertension, and atrial fibrillation. Moreover, chronic insomnia elevates the risk of major depressive disorder through persistent alterations in the hypothalamic‑pituitary‑adrenal axis. Treatment strategies must therefore be tailored: cognitive‑behavioral therapy for insomnia, CPAP for apnea, and orexin agonists for narcolepsy have demonstrated efficacy in controlled trials. Lifestyle modifications, such as maintaining a consistent bedtime, limiting blue‑light exposure, and avoiding caffeine after noon, reinforce the therapeutic effect of any medical intervention. Finally, regular screening for sleep disturbances in primary care can catch maladaptive patterns before they progress to systemic disease.
xie teresa
October 19, 2025 AT 07:58I hear you, and I want to add that the emotional toll of chronic sleep loss often goes unnoticed until it starts affecting relationships and work performance. Practicing mindfulness before bed can calm the nervous system and reduce the cortisol spikes you mentioned. Even a brief 5‑minute breathing exercise has been shown to increase sleep efficiency in otherwise healthy adults.
Srinivasa Kadiyala
October 24, 2025 AT 03:28While the article presents a solid overview, it neglects to mention that not all screen time is detrimental; some individuals actually find relaxation in reading e‑books with night‑mode enabled, which can, in fact, aid the transition to sleep, provided the content is not stimulating.
Alex LaMere
October 28, 2025 AT 21:58Sleep hygiene matters-keep the room dark, cool, and quiet 😴
Dominic Ferraro
November 2, 2025 AT 17:28Imagine waking up feeling refreshed as if you’d been kissed by a gentle sunrise; that’s what consistent sleep can gift you, and you have the power to claim it by simply honoring your body’s natural rhythms!
Jessica Homet
November 7, 2025 AT 12:58Great summary.
KayLee Voir
November 12, 2025 AT 08:28It’s encouraging to see you acknowledge the basics; remember, small incremental changes often stick better than sweeping overhauls, so start with one habit this week and build from there.
Bailey Granstrom
November 17, 2025 AT 03:58Don’t underestimate the cascade-one missed REM cycle can feel like a day lost in fog!
Melissa Corley
November 21, 2025 AT 23:28i think u should try less coffee after noon maybe its a thing 😂👍
Kayla Rayburn
November 26, 2025 AT 18:58That’s a valid point, and adding a short power nap can actually boost alertness without hurting your nighttime schedule, as long as you keep it under twenty minutes.
Jack Marsh
December 1, 2025 AT 14:28The exposition, while comprehensive, would benefit from a clearer delineation between pathophysiology and therapeutic recommendations, thereby enhancing readability for clinicians seeking quick reference.
Terry Lim
December 6, 2025 AT 09:58Specifically, the section on CPAP lacks cost considerations, which are pivotal for patient adherence.
Cayla Orahood
December 11, 2025 AT 05:28One must wonder whether the pharmaceutical industry is quietly steering the narrative toward medication-heavy solutions, subtly downplaying the profound impact of simple lifestyle adjustments.
McKenna Baldock
December 16, 2025 AT 00:58Sleep, in its quiet rhythm, mirrors the cycles of existence; by honoring its cadence we align ourselves with a deeper order that transcends mere physiological necessity.
Roger Wing
December 20, 2025 AT 20:28sure but the article misses the fact that cultural habits like siestas can actually improve overall sleep quality if done right
Matt Cress
December 25, 2025 AT 15:58Oh great another “just sleep more” article, because obviously we all have the luxury of ignoring work deadlines and Netflix binges, right?
Andy Williams
December 30, 2025 AT 11:28Indeed, evidence supports that consistent sleep timing reduces metabolic disturbances.