SSRI-Anticoagulant Bleeding Risk Calculator
Bleeding Risk Calculator
Calculate increased bleeding risk when combining SSRIs with anticoagulants based on anticoagulant class and therapy duration.
Input Parameters
Risk Assessment
Enter parameters above to see risk assessment
Monitoring Recommendations
Select an anticoagulant and duration to see monitoring recommendations
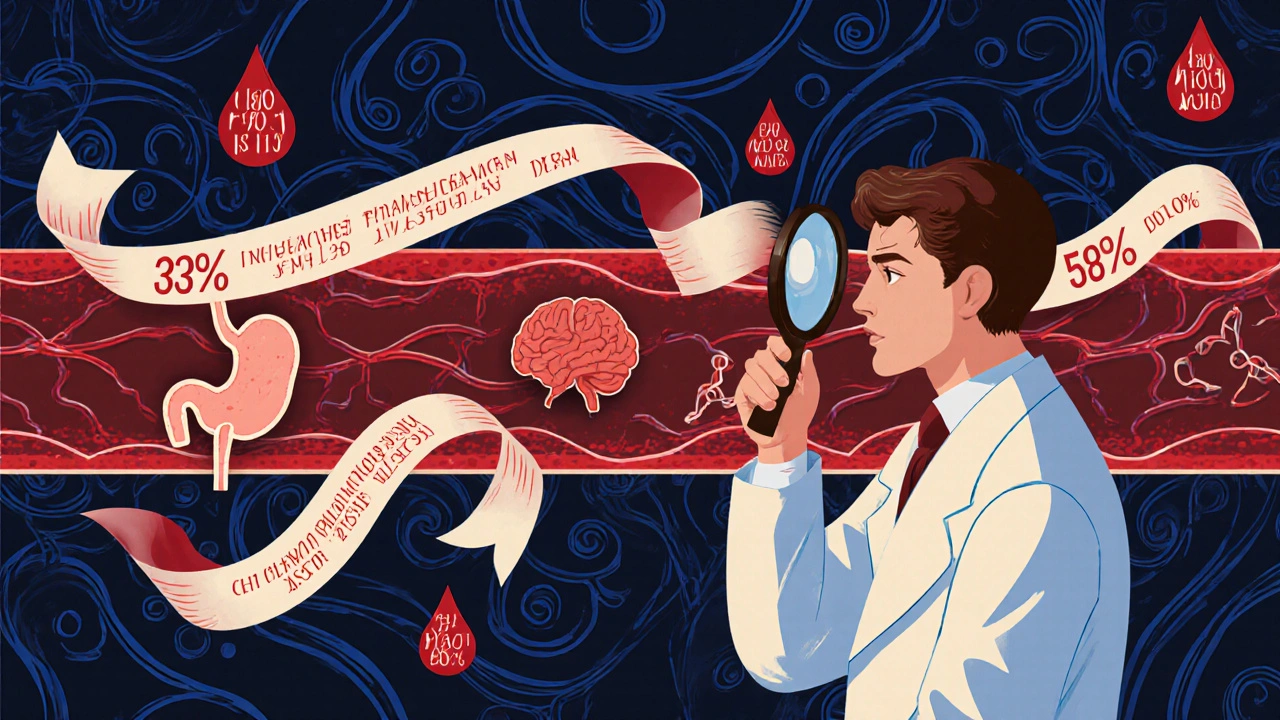
When you hear “SSRIs are selective serotonin reuptake inhibitors, a class of antidepressants that increase serotonin levels in the brain” and “Anticoagulants are medications that reduce blood clot formation, commonly prescribed for atrial fibrillation, deep‑vein thrombosis, and other clot‑prone conditions,” you might not immediately think they belong together. Yet clinicians are seeing more patients on both, and a growing body of research shows a real bleeding risk when the two are combined. Let’s break down why platelets matter, what the numbers say, and how to keep patients safe.
Why Platelets and Serotonin Matter
Platelets don’t make serotonin themselves; they borrow it from the bloodstream. Inside a platelet, serotonin acts like a signal that boosts the clotting response. SSRIs block the serotonin reuptake transporter, which also exists on platelets. The result? Platelets end up with 90% less serotonin at therapeutic SSRI doses, and laboratory tests show a 30‑40% drop in aggregation ability. In plain terms, the “glue” that seals tiny wounds is weaker, and that weakness becomes critical when a patient is also on an anticoagulant that already slows clot formation.
What the Latest Studies Show
The most comprehensive data comes from a 2024 JAMA Network Open analysis of 42,190 major‑bleeding cases matched to over a million controls. Patients on both an oral anticoagulant (OAC) and an SSRI faced a 33% higher incidence of major bleeding than those on an OAC alone (incidence rate ratio = 1.33; 95% CI 1.24‑1.42). The risk peaked in the first 30 days of combined therapy-roughly six additional bleeding events per 1,000 patient‑years-and tapered off after six months.
Older work by Sinno (2003) first linked SSRIs to platelet dysfunction, but newer studies have refined the picture. A 2025 in‑vitro study by Mokhtarian et al. showed that citalopram does not change standard coagulation times (e.g., lag time = 4.94 ± 0.95 min), confirming the problem is platelet‑centric, not a direct coagulation factor effect.
Bleeding Sites and Absolute Numbers
Not all bleeds are created equal. Gastrointestinal bleeding accounts for 58% of the combined‑therapy events (IRR = 1.35), intracranial hemorrhage makes up 17% (IRR = 1.28), and other major sites cover the remaining 25% (IRR = 1.31). In absolute terms, the event rate climbs from 1.8 per 100 person‑years with an OAC alone to 2.4 per 100 person‑years when an SSRI is added.
Do All Anticoagulants Carry the Same Risk?
When you split the data by anticoagulant class, a subtle pattern emerges. Vitamin K antagonists (VKAs) like warfarin show a 28% relative increase in bleeding (IRR = 1.28) compared with a 22% rise for direct oral anticoagulants (DOACs) such as apixaban or rivaroxaban. The difference isn’t statistically decisive, but it hints that DOACs may be the safer option if an SSRI is unavoidable.
Does the Choice of SSRI Matter?
One might expect a high‑potency SSRI like paroxetine to create more bleeding than a milder agent such as escitalopram. The Rahman cohort found no meaningful divergence-both drugs produced an IRR of about 1.33. Real‑world prescribing patterns echo this finding: sertraline dominates the market (about 52% of SSRI prescriptions in anticoagulated patients) because its pharmacokinetic profile is relatively benign, not because it lowers bleeding risk.
Clinical Guidelines and Expert Opinions
The American Heart Association (AHA) issued its first guidance on this interaction in 2017, and the FDA added a label warning in 2019 after 27 serious post‑marketing bleeding reports. Yet experts still disagree on how cautious we should be. Dr. Allison Rahman, senior author of the JAMA study, urges “close monitoring, especially during the first few months,” while Dr. Gregory Quinn, who analyzed the ROCKET‑AF trial, argues that “the data provide reassurance that SSRIs can be safely added in most atrial‑fibrillation patients.” The American Psychiatric Association’s 2022 guideline lands in the middle, recommending alternative antidepressants for high‑bleeding‑risk patients but not calling for an outright ban.
How to Manage the Risk in Practice
Here’s a quick checklist you can use in a primary‑care or cardiology clinic:
- Screen every new anticoagulant patient for depression or anxiety; if present, consider non‑SSRI options such as mirtazapine or bupropion for those with a HAS‑BLEED score ≥ 3.
- If an SSRI is essential, choose sertraline or escitalopram as first‑line choices.
- For warfarin users, double the INR monitoring frequency during the first month of combined therapy (e.g., twice weekly).
- Order a baseline complete blood count (CBC) and fecal occult blood test, then repeat the CBC monthly for three months.
- Educate patients on warning signs: black or tarry stools, unexplained bruising, sudden headache, or weakness.
These steps line up with the American Academy of Family Physicians’ Choosing Wisely recommendation that 68% of inappropriate SSRI‑anticoagulant combos happen in primary care, often because the bleed‑risk assessment is missed.

Comparison of Bleeding Risk by Anticoagulant Class
| Anticoagulant Class | Relative Risk (IRR) | 95% CI | Typical Monitoring |
|---|---|---|---|
| Vitamin K antagonists (warfarin) | 1.28 | 1.15‑1.42 | INR twice weekly (first month) |
| Direct oral anticoagulants (apixaban, rivaroxaban, dabigatran) | 1.22 | 1.08‑1.38 | Renal function & drug‑specific labs quarterly |
| No anticoagulant (control) | 1.00 | - | - |
The table underscores that while the absolute increase is modest, it is consistent across classes. That consistency is why most guidelines treat the interaction as a class effect rather than a drug‑specific warning.
Economic Impact and Why It Matters
In the United States, a major bleeding episode costs roughly $18,750 on average. With an estimated 1.2 billion dollars spent annually on preventable SSRI‑anticoagulant‑related bleeds, even small improvements in prescribing habits can save millions. The cost argument aligns with the 2025 FDA label update that urges clinicians to weigh non‑SSRI options when additional bleeding risk factors are present.
Future Research and Decision‑Support Tools
The PRECISION‑AF trial (NCT04892043) is currently enrolling 5,000 patients to compare bleeding outcomes between SSRI and non‑SSRI antidepressants in anticoagulated atrial‑fibrillation. Results are due in late 2026 and could finally settle the controversy. Meanwhile, the American College of Cardiology is developing a clinical‑decision‑support algorithm that blends HAS‑BLEED scores with depression severity scales, aiming to suggest the safest antidepressant at the point of care.
Until those tools are ready, the best strategy remains a blend of good data, patient‑centered conversation, and diligent monitoring.
Key Take‑aways
- SSRIs lower platelet serotonin, weakening clot formation.
- Combined SSRI‑anticoagulant therapy raises major bleeding risk by about 33%, especially in the first month.
- DOACs may be slightly safer than warfarin, but the risk increase exists for all anticoagulants.
- Choose sertraline or escitalopram if an SSRI is needed, and consider non‑SSRI alternatives for high‑risk patients.
- Baseline labs, frequent INR checks (for warfarin), and patient education are the cornerstones of safe management.
Does taking an SSRI with a DOAC require dose adjustment?
No current guidelines recommend changing the DOAC dose solely because of an SSRI. The focus is on monitoring and choosing an SSRI with a lower interaction profile.
What are the early signs of major bleeding I should watch for?
Look for black or tarry stools, vomiting blood, sudden severe headache, weakness or numbness, and unexplained bruising. If any appear, seek medical help right away.
Can I switch from warfarin to a DOAC to lower bleeding risk while on an SSRI?
Switching may reduce the relative increase in bleeding, but the decision must consider renal function, drug‑drug interactions, and the underlying indication for anticoagulation.
Is sertraline truly safer than other SSRIs when combined with anticoagulants?
Sertraline is preferred mainly because it has fewer cytochrome P450 interactions, not because it lowers platelet‑related bleeding risk more than other SSRIs.
How often should I get blood work if I’m on both an SSRI and warfarin?
During the first month, check INR twice weekly and complete blood count monthly. After three months, move to standard INR monitoring intervals unless problems arise.





christine badilla
October 25, 2025 AT 18:56I swear, watching a patient bleed because of a perfectly reasonable prescription is like watching a tragedy unfold on stage. The blood that should clot becomes a runaway river, spilling over every expectation. SSRIs silently rob platelets of serotonin, the very glue that seals a cut, and anticoagulants turn that glue into a weak paste. When the two meet, it isn’t a subtle whisper; it’s a deafening crash of physiology. The JAMA 2024 analysis reads like a cautionary tale, a 33% jump in major bleeding that screams for attention. Even the first month, those six extra events per 1,000 patient‑years feel like a relentless tide. Older studies that hinted at the danger now have a new, louder voice, and we can’t ignore it. Platelet aggregation drops 30‑40%, a number that no clinician should brush off as trivial. The brain may be happy with more serotonin, but the body pays a hidden price.
Warfarin users may notice an INR spike, while those on DOACs feel a subtler shift that still matters. Sertraline, the market darling, isn’t a magic bullet; it simply avoids extra cytochrome drama, not bleeding. The guidelines from AHA and FDA are clear, yet the field remains divided, with some experts waving flags of reassurance while others hoist warnings. A practical checklist, as you outlined, becomes a lifeline in this storm. Baseline CBCs, fecal occult tests, and patient education are not just paperwork; they are the barricades against disaster. We must remember that each bruise, each tarry stool, could be the first sign of a larger calamity.
In the end, the decision to pair an SSRI with an anticoagulant is a tightrope walk between mental health and hematologic safety. The cost of a bleed, both human and economic, is staggering. Better prescribing habits, vigilant monitoring, and patient dialogue are the three pillars that can keep us from falling off that rope. Let’s not let the serotonin surge blind us to the bleeding tide.
Pamela Clark
October 31, 2025 AT 17:56Oh great, another "groundbreaking" study confirming what the bedside nurse has been shouting for years. Because we definitely needed a fancy number to tell us bleeding is bad.
Diane Holding
November 6, 2025 AT 17:56The platelet serotonin pathway is often overlooked but crucial for hemostasis.
Screening for depression before starting anticoagulation can catch this risk early.
Manish Verma
November 12, 2025 AT 17:56Exactly, and adding a simple CBC can flag problems before they become catastrophic.
Patients love a quick blood test if it means fewer scary ER visits.
Greg Galivan
November 18, 2025 AT 17:56Look folks these data are clear dont ignore the bleed risk its real and serious.
Doctors need to act now not later.
Kala Rani
November 24, 2025 AT 17:56Honestly I think the whole thing is overhyped there is no real danger
Donal Hinely
November 30, 2025 AT 17:56Mate if you’re going to sprinkle serotonin blockers on a blood‑thin patient you might as well hand them a chainsaw.
The risk isn’t subtle, it’s a full‑blown avalanche.
eko lennon
December 6, 2025 AT 17:56Let me break this down for everyone who’s still scrolling past the abstract. First, the biology: platelets hijack serotonin from the plasma to amplify their clotting response, acting like a tiny alarm system that tells the rest of the clotting cascade to step up. When an SSRI is introduced, that alarm is muffled; platelets lose up to 90% of their serotonin payload, which translates to a measurable dip in aggregation capacity. Second, the epidemiology: the 2024 JAMA Network Open study you cited pooled over 42,000 major‑bleeding events and found a 33% relative increase when an oral anticoagulant meets an SSRI. That isn’t a marginal figure-it’s a substantial shift, especially in the critical first 30‑day window where the absolute risk jumps by six events per 1,000 patient‑years.
Third, the drug‑class nuance: warfarin users see a 28% bump versus a 22% rise with DOACs. The confidence intervals overlap, but the trend hints that DOACs might be the slightly safer playground if you can’t ditch the SSRI. Fourth, the clinical action: baseline labs (CBC, fecal occult blood) and intensified INR monitoring for warfarin (twice weekly for the first month) are low‑cost safeguards that can catch early drops in hemoglobin before a catastrophic bleed erupts. Fifth, the patient‑focused angle: educate on black tarry stools, unexplained bruising, and sudden headaches-these are the red flags that every primary‑care physician should weave into the discharge paperwork.
Lastly, the future: the PRECISION‑AF trial is gearing up to compare SSRI versus non‑SSRI antidepressants in anticoagulated atrial‑fibrillation patients, and the ACC’s decision‑support algorithm aims to marry HAS‑BLEED scores with depression severity scales. Until those tools are live, we have to rely on good old‑fashioned vigilance, shared decision‑making, and the checklist you laid out. In short: the data are clear, the risk is real, and the mitigation steps are straightforward-use them.
Sunita Basnet
December 12, 2025 AT 17:56You nailed it - the evidence base is solid and the clinical implications are crystal clear.
Implementing baseline CBCs and patient education can dramatically cut preventable bleeds.
Melody Barton
December 18, 2025 AT 17:56Just stop the combo.
Justin Scherer
December 24, 2025 AT 17:56I wonder how much renal function plays into the decision‑making for DOACs plus SSRIs.
Perhaps more real‑world data will clarify the risk gradient.
Cheyanne Moxley
December 30, 2025 AT 17:56Putting patients at unnecessary risk is downright unethical.
Kevin Stratton
January 5, 2026 AT 17:56In the end, medicine is a balance between art and science 😊.
We must weigh freedom of mental health treatment against corporeal safety.
ALBERT HENDERSHOT JR.
January 11, 2026 AT 17:56Your summary captures the nuances admirably.
Implementing the checklist could indeed mitigate many adverse events.
Thank you for compiling such a thorough overview.