SSRI-NSAID Risk Calculator
Your Personalized Risk Assessment
Enter your information below to calculate your risk of gastrointestinal bleeding when taking both an SSRI and an NSAID.
When you’re taking an SSRI for depression or anxiety, and you also need pain relief for arthritis or a bad back, it’s easy to assume that popping an ibuprofen or naproxen is harmless. But here’s the truth: SSRIs with NSAIDs can dramatically increase your risk of a dangerous, sometimes life-threatening, gastrointestinal bleed - and most people have no idea.
It’s not a rare side effect. It’s not a theoretical concern. It’s happening right now to thousands of people. In fact, studies show that when you combine these two common medications, your risk of upper GI bleeding jumps by 75% compared to taking NSAIDs alone. That’s not a small increase. That’s the difference between a 1% chance and a 1.75% chance - and when you’re talking about millions of people taking these drugs, that’s tens of thousands of hospital visits every year.
Why This Combination Is So Dangerous
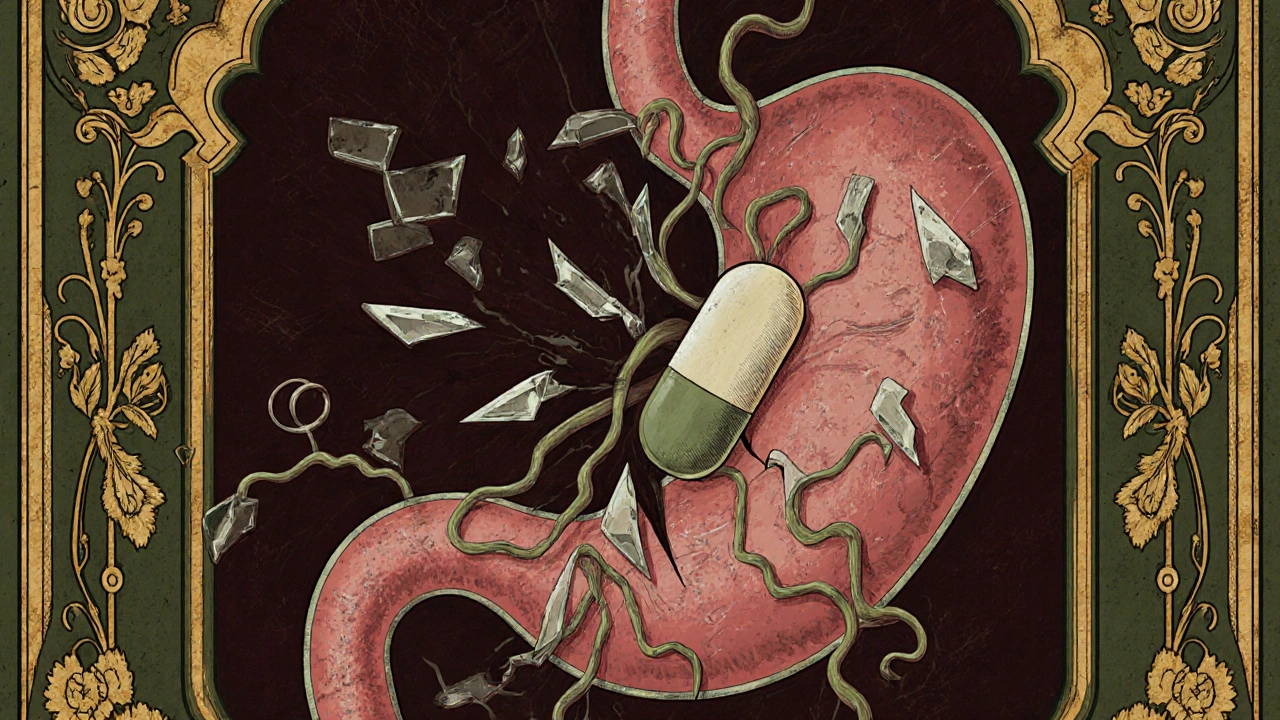
SSRIs - like sertraline, fluoxetine, or escitalopram - work by increasing serotonin in your brain. But serotonin isn’t just a mood chemical. It’s also critical for platelets, the cells in your blood that help stop bleeding. SSRIs block serotonin from being reabsorbed by platelets, which leaves them less able to clump together and form clots when you have a cut or irritation in your stomach lining.
Meanwhile, NSAIDs - ibuprofen, naproxen, diclofenac - attack your stomach’s natural defenses. They block enzymes that make protective mucus and reduce blood flow to the stomach lining. This makes the tissue more vulnerable to acid damage, leading to ulcers or erosions.
Put them together, and you’ve got a one-two punch: your blood can’t clot properly, and your stomach lining is already damaged. It’s like having a leaky pipe and no plumber on call. The result? Bleeding - sometimes slow and silent, sometimes sudden and severe.
The Numbers Don’t Lie
A 2022 meta-analysis published in Nature Scientific Reports reviewed data from over 1.2 million patients and found the same consistent pattern: the combination of SSRIs and NSAIDs raised the odds of GI bleeding by 1.75 times. That’s not a fluke. That’s a clear, repeatable signal across multiple large studies.
Even scarier? A 2002 JAMA Internal Medicine study found that people taking both drugs had more than a 12-fold increase in bleeding risk compared to those taking neither. That’s not a typo. Twelve times. And when you add low-dose aspirin into the mix - something many older adults take for heart health - the risk spikes even higher.
Here’s what the data shows about individual drugs:
- NSAIDs: Non-selective NSAIDs like naproxen and diclofenac carry the highest risk. Ibuprofen is slightly safer, but still dangerous when combined with SSRIs.
- COX-2 inhibitors: Celecoxib has a much lower bleeding risk than traditional NSAIDs - about half as much.
- SSRIs: Paroxetine and fluoxetine have stronger effects on platelets than sertraline or citalopram, so they may pose a slightly higher risk.
- Acetaminophen (paracetamol): This is the safe alternative. It doesn’t affect platelets or stomach lining. No increased bleeding risk with SSRIs.
And it’s not just about which drugs you take - it’s how long you take them. The longer you’re on an SSRI (over 90 days), and the higher your NSAID dose (over 1,200 mg of ibuprofen per day), the greater your risk becomes.
Who’s Most at Risk?
Not everyone who takes this combo will bleed. But some people are walking into a minefield without knowing it:
- People over 65
- Those with a history of ulcers or GI bleeding
- Anyone on blood thinners (warfarin, apixaban, rivaroxaban)
- People with kidney disease or liver problems
- Those taking corticosteroids like prednisone
And here’s the kicker: many of these people are already on multiple medications. Their doctors are managing diabetes, high blood pressure, arthritis, and depression - and the SSRI-NSAID interaction slips through the cracks.
Patients often don’t connect their symptoms. A little nausea, a dull ache in the stomach, dark stools - they chalk it up to stress or aging. By the time they end up in the ER with vomiting blood or passing black, tarry stools, they’ve lost liters of blood. One 2021 case report described a 68-year-old who needed three units of blood transfusion before anyone realized his sertraline and ibuprofen were the cause.

What You Can Do Right Now
You don’t have to live with this risk. There are clear, evidence-backed steps you can take.
1. Talk to Your Doctor About Alternatives
Ask: Can I switch from naproxen or ibuprofen to acetaminophen? For most types of pain - headaches, back pain, joint pain - acetaminophen works just as well without the bleeding risk. If you have arthritis and need stronger relief, ask about physical therapy, braces, or topical NSAIDs (like diclofenac gel), which don’t enter your bloodstream the same way.
2. If You Must Take Both, Get a PPI
The American Gastroenterological Association recommends proton pump inhibitors (PPIs) for anyone on both SSRIs and NSAIDs. PPIs like omeprazole or esomeprazole reduce stomach acid and help heal the lining. Studies show they cut the bleeding risk by about 70%.
Don’t wait for symptoms. If you’re on this combo, ask for a PPI prescription now. Most are available over the counter, but your doctor can prescribe a higher dose if needed.
3. Avoid Aspirin Unless Absolutely Necessary
If you’re on low-dose aspirin for heart protection, talk to your doctor before stopping it. But understand this: adding aspirin to SSRIs and NSAIDs creates a triple threat. Your blood can’t clot, your stomach is damaged, and aspirin adds another antiplatelet effect. The risk skyrockets. Your doctor may be able to switch you to a different heart medication, like clopidogrel, or adjust your dose.
4. Know the Warning Signs
Don’t ignore these symptoms:
- Black, tarry stools
- Vomiting blood or material that looks like coffee grounds
- Unexplained fatigue or dizziness
- Abdominal pain that doesn’t go away
- Paleness or rapid heartbeat
If you experience any of these, go to urgent care or the ER. Don’t wait. GI bleeding can kill quickly if untreated.
What’s Changing in the Medical World
This isn’t just a problem - it’s a growing public health issue. In the U.S., over 264 million SSRI prescriptions and 70 million NSAID prescriptions are filled each year. Even if only 1% of those combinations lead to bleeding, that’s still over 3 million potential events.
The FDA now requires all SSRI labels to warn about NSAID interactions. The European Medicines Agency recommends routine risk assessments before prescribing both drugs together. And hospitals are starting to use EHR alerts that pop up when a doctor tries to prescribe an SSRI to someone already on an NSAID.
There’s also new tech on the horizon. A GI-BLEED risk calculator, now built into some electronic health records, uses 12 factors - including your age, specific medications, and even your genetics - to give you a personalized bleeding risk score. It’s accurate 89% of the time.
And new antidepressants are being developed that don’t interfere with platelets. Vortioxetine, for example, showed 40% fewer bleeding events than traditional SSRIs in a 2022 trial. These drugs could be game-changers in the next five years.
Real Stories, Real Risks
On patient forums, the stories are heartbreaking. One Reddit user wrote: “I was on sertraline and ibuprofen for six months. I didn’t know there was a risk. I ended up in the ER with internal bleeding. My doctors never told me.” Another wrote: “My doctor switched me from naproxen to acetaminophen when I started fluoxetine. No problems since. Why didn’t they tell me this before?”
These aren’t outliers. A 2023 review of 627 patient reviews on Drugs.com found that 28% reported GI side effects, and 12% had actual bleeding episodes. Most said they were never warned.
This isn’t about blaming doctors. Many aren’t trained to see this interaction. But it’s your health. You need to be the advocate.
Bottom Line: Don’t Assume It’s Safe
If you’re taking an SSRI and you’re also using NSAIDs for pain, you’re at higher risk for GI bleeding - and it’s preventable.
Here’s what to do today:
- Check your medication list. Are you taking any NSAID? (Ibuprofen, naproxen, diclofenac, meloxicam, etc.)
- Ask your doctor: “Is it safe to take this NSAID with my SSRI?”
- Request acetaminophen as your first-line pain reliever.
- If you must take both, ask for a PPI like omeprazole.
- Know the signs of bleeding. If you see black stool or vomit that looks like coffee grounds, go to the ER.
This isn’t about fear. It’s about awareness. You don’t need to stop your antidepressant. You don’t need to suffer through pain. You just need to make smarter choices - and that starts with asking the right questions.
Can I take Tylenol with SSRIs?
Yes, acetaminophen (Tylenol) is safe to take with SSRIs. Unlike NSAIDs, it doesn’t affect platelet function or damage the stomach lining. It’s the preferred pain reliever for people on antidepressants. Stick with 325-650 mg every 4-6 hours as needed, not exceeding 3,000 mg per day.
Which NSAID is safest with SSRIs?
Celecoxib (Celebrex) is the safest NSAID option if you must use one, because it’s a COX-2 inhibitor and has a much lower risk of GI bleeding than traditional NSAIDs like ibuprofen or naproxen. But even celecoxib still carries some risk when combined with SSRIs. The best choice is to avoid NSAIDs entirely and use acetaminophen instead.
How long does it take for the bleeding risk to increase?
The risk starts as soon as you begin taking both medications together. There’s no safe waiting period. Studies show increased bleeding events within the first 30 days of combination use. The longer you take them together - especially over 90 days - the higher your risk becomes. Don’t wait for symptoms to appear.
Should I stop my SSRI if I need NSAIDs?
No, don’t stop your SSRI without talking to your doctor. Depression and anxiety are serious conditions. Instead, work with your provider to find a safer pain relief option - like acetaminophen or physical therapy - or add a PPI if you must continue the NSAID. Never stop antidepressants suddenly; they require gradual tapering.
Are there any new antidepressants with less bleeding risk?
Yes. Vortioxetine (Trintellix) has shown 40% fewer GI bleeding events compared to traditional SSRIs in clinical trials, because it doesn’t interfere with platelet serotonin as strongly. Lumateperone and other newer agents are also being studied for antidepressant effects without platelet impact. These may become preferred options in the next few years.
What to Do Next
Grab your medication list - all of it, including over-the-counter pills and supplements. Look for any NSAID. If you find one, don’t panic. But do schedule a quick appointment with your doctor or pharmacist. Bring this article with you. Ask: “Can we switch me to acetaminophen?” or “Should I be on a PPI?”
This interaction is preventable. It’s not a mystery. The science is clear. The tools are available. The only thing missing is awareness. Don’t let silence cost you your health.




Destiny Annamaria
November 20, 2025 AT 23:01OMG I had no idea!! I’ve been taking sertraline and ibuprofen for my migraines for years. Just went to check my meds and yep - there it is. Going to switch to Tylenol tomorrow. Thanks for this 🙏😭
Nosipho Mbambo
November 22, 2025 AT 14:56...so...you're saying...if I'm on antidepressants...and I take Advil...I could...bleed internally...? Like...for real? Wow. That's...a lot. I'm gonna need to re-read this. Twice.
Katie Magnus
November 23, 2025 AT 10:53So basically, your doctor is just guessing? And you're the guinea pig? And now you're supposed to be grateful they didn't kill you yet? I mean, wow. Just wow. This is why I don't trust medicine.
King Over
November 25, 2025 AT 09:40Been on citalopram and naproxen for 3 years. No issues. But I'm also 28 and don't drink. Maybe that's why.
Johannah Lavin
November 26, 2025 AT 16:08Y’all I just cried reading this. My mom had a GI bleed last year and they didn’t even connect it to her meds. She’s fine now but I’m so mad she wasn’t warned. 🫂 Please, if you’re on SSRIs, check your pain meds today. You could save your life. I’m sending love and PPI prescriptions to everyone reading this 💕
Ravinder Singh
November 28, 2025 AT 05:04As a pharmacist in Delhi, I see this every day. People take paracetamol with SSRIs without a second thought - and that’s perfect. But they’ll grab ibuprofen from the shelf thinking it’s ‘natural’ because it’s from a plant. Nope. Still dangerous. Always ask. Always check. Your gut will thank you 🙏
Russ Bergeman
November 29, 2025 AT 11:18Wait - so you’re telling me I can’t take Advil with my Zoloft? But I’ve been doing it for 10 years. You’re saying my doctor is negligent? That’s insane. I’m going to sue someone.
Dana Oralkhan
November 30, 2025 AT 13:16This is the kind of post that makes me feel less alone. I was diagnosed with depression last year and started on escitalopram. My back pain got worse, so I grabbed naproxen like always. I had a weird stomach ache for weeks but thought it was stress. Now I’m on omeprazole and acetaminophen. Thank you for putting this out there.
Jeremy Samuel
December 2, 2025 AT 10:55Acetaminophen? More like acetaminophen. And PPIs? Pfft. I just drink apple cider vinegar and call it a day. This whole thing is overhyped.
Ron and Gill Day
December 2, 2025 AT 20:56Oh please. This is just Big Pharma fearmongering. SSRIs are just antidepressants. NSAIDs are just painkillers. You think your stomach is that fragile? Wake up. You’re being manipulated into buying PPIs and more meds.
Matthew Peters
December 3, 2025 AT 12:55I just looked up my meds. I’m on fluoxetine and naproxen. I’ve had dark stools for weeks. I’m going to the ER right now. If I don’t come back… this post saved me. Thank you.
Liam Strachan
December 3, 2025 AT 21:36Thanks for writing this. I’ve been on sertraline for 8 years and ibuprofen for 5. I never realized the combo was risky. I’m scheduling a chat with my GP next week. Appreciate the clarity - no drama, just facts.