Managing diabetes isn’t just about checking blood sugar levels. It’s about understanding the medicines you’re taking, why they work, and what your body might do in response. If you’ve been prescribed a diabetes medication-or are considering one-you’re probably wondering: What side effects should I expect? And more importantly, how do I handle them without giving up on my treatment?
Metformin: The First Line, But Not Always Easy
Most people with type 2 diabetes start with metformin. It’s cheap, effective, and doesn’t cause weight gain or low blood sugar. But for about 1 in 3 people, it brings stomach trouble. Nausea, diarrhea, bloating-these aren’t rare. In fact, a 2021 JAMA study found 26% of users had nausea, and 23% had diarrhea. That’s why many quit within the first month.
The trick? Start low. Take 500 mg once a day with dinner. Give your body a week to adjust. Then slowly increase. Switching to the extended-release version cuts GI side effects by half. And if you’re on metformin for more than five years, get your vitamin B12 checked. Up to 30% of long-term users become deficient, which can cause fatigue, numbness, or even memory problems. A simple monthly B12 shot fixes it in most cases.
Sulfonylureas: Effective, But Risky
Drugs like glyburide and glipizide force your pancreas to pump out more insulin. They work fast and are inexpensive. But they come with a big catch: low blood sugar. About 1 in 6 people on these meds have at least one serious low blood sugar episode every year. That means shaking, sweating, confusion-even passing out. And if you skip a meal? Risk jumps 3.2 times.
They also cause weight gain-usually 2 to 4 kg. That’s the opposite of what most people with type 2 diabetes need. Many patients switch away from these drugs once they learn about safer options. If you’re on one and feel shaky between meals, talk to your doctor. You might be able to move to something that doesn’t force your pancreas to overwork.
Thiazolidinediones: Weight Gain and Heart Risks
Pioglitazone (Actos) makes your body respond better to insulin. But it also makes your body hold onto water. About 5% of users get swollen ankles or shortness of breath-signs your heart is under strain. The PROactive trial showed a 43% higher risk of heart failure with this class. Weight gain is common too, averaging 2-3 kg. Because of this, doctors rarely prescribe these anymore unless other options have failed.
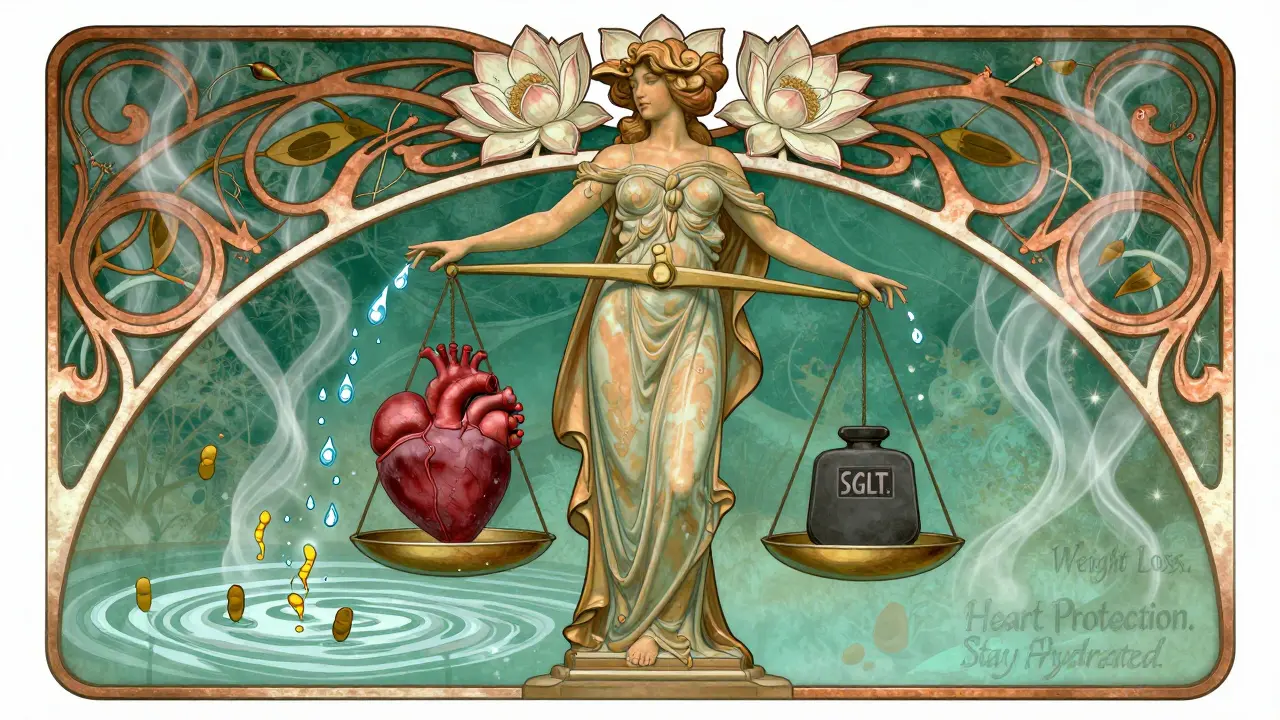
SGLT2 Inhibitors: Losing Weight, Gaining Infections
Drugs like dapagliflozin (Farxiga) and empagliflozin (Jardiance) make your kidneys flush out sugar through urine. The result? Lower blood sugar, weight loss, and lower risk of heart and kidney damage. In fact, studies show they cut heart failure hospitalizations by up to 30%.
But there’s a downside. You’re peeing out glucose-and that sugar feeds yeast. Up to 15% of women and 5% of men get genital yeast infections. It’s not dangerous, but it’s annoying. Daily washing, cotton underwear, and avoiding douches can cut recurrence by 60%. You might also get more urinary tract infections or feel dizzy if you’re dehydrated. Drink more water. And watch for signs of ketoacidosis: nausea, vomiting, stomach pain, and fruity-smelling breath. It’s rare-under 0.3% of users-but serious.
GLP-1 Receptor Agonists: Weight Loss with Nausea
Liraglutide (Victoza), semaglutide (Ozempic), and tirzepatide (Mounjaro) are game-changers. They mimic a gut hormone that slows digestion, reduces appetite, and boosts insulin when needed. People lose 5-10 kg on average. Many report better blood sugar control and fewer cravings.
But nausea hits 30-50% of users. Vomiting and diarrhea are common too. Most side effects fade after a few weeks. Start with the lowest dose. Wait four weeks before increasing. If you can’t tolerate it, don’t give up-ask about switching to the once-weekly version. It’s often easier on the stomach. And if you’re on one of these and feel unusually tired or have persistent vomiting, get checked. There’s a small risk of pancreatitis or gallbladder problems.
Insulin: The Most Powerful, But Most Complex
Insulin is essential for type 1 diabetes and often needed in advanced type 2. But it’s the hardest to manage. The biggest fear? Low blood sugar. People on intensive insulin regimens can have 15-30 episodes a year. That’s why many intentionally skip doses to avoid lows. But that’s dangerous. Your blood sugar can spike and damage organs over time.
Weight gain is another issue. Most gain 2-5 kg. To manage this, pair insulin with lifestyle changes. And use a continuous glucose monitor (CGM). The DIAMOND trial showed CGMs cut severe lows by 40%. Learn the 15-15 rule: if your blood sugar drops below 4 mmol/L, eat 15 grams of fast-acting carbs (like juice or glucose tablets), wait 15 minutes, check again. Repeat if needed.
Newer Options and What’s Coming
Tirzepatide (Mounjaro), approved in 2022, combines two hormones (GIP and GLP-1) and causes more weight loss than older GLP-1 drugs-with less nausea. In trials, users lost up to 20% of their body weight. Oral GLP-1 pills like orforglipron are now in late-stage testing and could replace injections soon. Once-weekly basal insulin (icodec) is approved in Europe and may come to the U.S. soon.
But access remains a problem. While metformin costs $4 a month, newer drugs like Ozempic or Mounjaro can hit $900 without insurance. One in four Americans skip doses because of cost. Ask your doctor about patient assistance programs. Many drugmakers offer free or discounted meds if you qualify.
What to Do If Side Effects Hit
Don’t stop your meds without talking to your doctor. But don’t suffer in silence either. Keep a log: note what you’re taking, when you feel sick, and what helped. Bring it to your next appointment. Small tweaks-timing, dosage, switching formulations-can make a huge difference.
For metformin: take with food, switch to extended-release.
For SGLT2 inhibitors: drink water, wear cotton underwear, monitor for ketoacidosis.
For GLP-1 agonists: start low, go slow, don’t rush the dose increase.
For insulin: use a CGM, carry glucose tabs, teach someone how to help you during a low.
And if you’re worried about cost? Ask about generics. Ask about coupons. Ask about clinical trials. You’re not alone in this.
Final Thought: It’s Not One Size Fits All
There’s no perfect diabetes medication. What works for your neighbor might wreck your stomach. What keeps your friend’s blood sugar steady might make you gain weight. The goal isn’t to find the ‘best’ drug-it’s to find the right one for you. That means talking openly about side effects, costs, and lifestyle. Your doctor isn’t judging you. They’re trying to help you live better.
Diabetes treatment has come a long way since insulin was first discovered in 1921. Today, we have tools that don’t just control sugar-they protect your heart, kidneys, and quality of life. But only if you use them the right way. And that starts with knowing what to expect.
Can diabetes medications cause weight gain?
Yes, some can. Sulfonylureas and insulin commonly cause weight gain-usually 2 to 5 kg. Thiazolidinediones like pioglitazone also lead to fluid retention and weight gain. But newer drugs like SGLT2 inhibitors and GLP-1 receptor agonists often cause weight loss. Metformin is weight-neutral. Your choice of medication should match your goals: if losing weight is important, avoid drugs that make you gain it.
Why does metformin cause diarrhea?
Metformin affects gut bacteria and slows digestion, which can lead to bloating, gas, and loose stools. It’s not an allergy-it’s a side effect of how the drug works in the intestines. Taking it with food, starting with a low dose, or switching to the extended-release version can reduce these symptoms by up to 50%. Most people adjust within a few weeks.
Are SGLT2 inhibitors safe for people with kidney problems?
They’re often recommended. SGLT2 inhibitors like empagliflozin (Jardiance) and dapagliflozin (Farxiga) were originally developed for diabetes, but trials like EMPA-KIDNEY showed they protect the kidneys-even in people without diabetes. They reduce the risk of kidney failure and hospitalization for heart failure. Your doctor will check your eGFR before prescribing, but many patients with early-stage kidney disease benefit greatly.
Can I stop my diabetes medication if I lose weight?
Some people can-especially if they’ve lost a lot of weight and improved their diet and activity levels. But never stop without talking to your doctor. Stopping suddenly can cause blood sugar to spike. Your doctor may reduce your dose gradually while monitoring your HbA1c. Some patients stay off meds for years after significant lifestyle changes. Others need to restart later. It’s individual.
What’s the safest diabetes medication for older adults?
Metformin is usually safest for older adults without kidney issues. It doesn’t cause low blood sugar or weight gain. But if kidney function is low (eGFR below 30), insulin or GLP-1 agonists might be better. Avoid sulfonylureas in older patients-they increase fall risk from hypoglycemia. Always consider cognitive health, mobility, and ability to manage multiple doses. Simpler regimens reduce risk.
Do diabetes medications increase the risk of cancer?
No strong evidence links current diabetes medications to cancer. Early concerns about rosiglitazone (Avandia) and heart risk led to restrictions, but no cancer link was found. Studies on metformin even suggest it may lower cancer risk in some people. GLP-1 agonists and SGLT2 inhibitors have been monitored for over a decade with no increase in cancer rates. The FDA requires long-term safety data before approving new diabetes drugs, so current options are well-studied.
Why do I feel dizzy when I start an SGLT2 inhibitor?
SGLT2 inhibitors make you lose sugar and water through urine, which can lower blood volume and cause dehydration. Dizziness, especially when standing up, is a sign of low blood pressure from fluid loss. Drink more water-aim for 1.5-2 liters daily. Avoid alcohol and diuretics like coffee in excess. If dizziness continues after a week, talk to your doctor. You may need to lower the dose or switch.
Can I take diabetes meds during pregnancy?
Insulin is the safest choice during pregnancy. Metformin is sometimes used off-label and considered relatively safe (FDA Category B), but most other oral meds like sulfonylureas, SGLT2 inhibitors, and GLP-1 agonists are not recommended (Category C or D). Always plan ahead if you’re thinking of getting pregnant. Work with your doctor to switch to insulin before conception to keep blood sugar stable and protect the baby.
What’s Next?
If you’re struggling with side effects, you’re not failing. You’re just on the wrong path for your body. Talk to your doctor about alternatives. Ask about cost. Ask about lifestyle support. Ask if you can try a different drug for a month. Most side effects are manageable. Most are temporary. And most can be fixed with the right adjustment.
Diabetes treatment isn’t about perfection. It’s about progress. The right medication doesn’t just lower your numbers-it gives you back your life. But only if you know what to expect, and how to respond when things go sideways.







franklin hillary
February 2, 2026 AT 04:40Let me tell you something real - diabetes meds aren’t magic pills, they’re tools. And like any tool, you gotta learn how to use ‘em right. I’ve seen people quit metformin after three days because their stomach felt like a washing machine on spin cycle. But here’s the thing - they didn’t start low. They didn’t go slow. They didn’t switch to ER. Now they’re back on insulin and wondering why they’re tired all the time. The answer? Patience. And maybe a little education.
GLP-1s? Yeah they cause nausea. So what? So does pregnancy. You don’t quit pregnancy because you puke in week 4. You adjust. You hydrate. You wait. And then boom - your cravings vanish, your A1c drops, and you forget what a bagel tastes like. That’s not a side effect, that’s a lifestyle upgrade.
And don’t get me started on cost. $900 for Ozempic? That’s a crime. But guess what? There are patient programs. There are coupons. There are generics coming. You don’t have to be rich to take care of yourself. You just have to be stubborn enough to ask for help.
This isn’t about perfection. It’s about progress. One pill. One day. One better choice at a time. You’re not broken. You’re just learning.
Naomi Walsh
February 3, 2026 AT 09:00How quaint. You all treat diabetes like it’s a minor inconvenience you can ‘manage’ with a few lifestyle tweaks and a coupon code. The reality? Most of these drugs are designed for obese, sedentary Americans who think ‘eating salad’ counts as discipline. Metformin’s GI side effects? That’s just your gut screaming because you’ve been feeding it processed carbs for 20 years. The real issue isn’t the medication - it’s the culture of denial that treats type 2 diabetes as a ‘lifestyle choice’ rather than a metabolic catastrophe. And yes, I’ve read the JAMA study. And no, you don’t get to call it ‘common’ and then act surprised when people can’t tolerate it. That’s not a side effect - that’s a symptom of systemic neglect.
And don’t even get me started on SGLT2 inhibitors. You call yeast infections ‘annoying’? Try explaining to your partner why you can’t have sex for six weeks because your body is literally fermenting sugar. And yes, I’ve had it. Twice. Because someone told me ‘drink more water’ like that’s a cure. It’s not. It’s a Band-Aid on a hemorrhage.
Meanwhile, the pharmaceutical industry is laughing all the way to the bank while you’re Googling ‘can you die from ketoacidosis?’
Nancy Nino
February 3, 2026 AT 16:39Oh, sweet summer child.
You really think the answer to diabetes is just ‘start low, go slow’? Darling, if you’re on insulin and skipping doses to avoid lows, you’re not being brave - you’re being terrified. And no amount of 15-15 rule pamphlets will fix that. The real problem? The system doesn’t give you the tools to live. It gives you a glucose meter and a prayer.
And yet - you still show up. You still log your numbers. You still fight. And for that? I salute you. Not with emojis. Not with memes. But with quiet, unshakable respect.
Lu Gao
February 3, 2026 AT 17:06Wait - so you’re telling me that a drug that makes you pee out sugar is supposed to be safe… but you still need to wear cotton underwear? 😂 I mean, I get it - yeast doesn’t care about your A1c. But honestly, if your medication turns your private life into a microbiology lab, maybe it’s time to ask: is this really worth it? Also, I just Googled ‘SGLT2 inhibitor and UTI’ and now I’m scared to drink water. 🤭
Jamie Allan Brown
February 5, 2026 AT 11:35I’ve been on metformin for 11 years. B12 deficiency? Yeah. Fatigue? Oh yeah. Numbness in my fingers? Three years ago, I thought it was carpal tunnel. Turns out, it was the drug. I started monthly shots. Within a month, I could type again. No drama. No panic. Just a simple fix that no one told me about until I googled ‘metformin and nerve damage’ at 2 a.m.
My point? Don’t assume your doctor knows everything. They’re human. They’re overwhelmed. But you? You’re the one living with this. So ask. Even if it feels awkward. Even if you think they’ll judge you. You’re not being a bother. You’re being smart.
And if you’re scared of side effects? You’re not alone. But you’re not powerless either.
Lisa Rodriguez
February 6, 2026 AT 13:50I switched from sulfonylureas to Jardiance and lost 14 pounds in 3 months. No gym. No diet. Just my kidneys doing the work. But then I got a yeast infection. And then another. And then my partner asked if I was ‘into that now.’ 😅 I started drinking cranberry juice, wearing cotton, and washing after every pee. It helped. Not perfect. But better. I wish someone had told me that before I cried in the pharmacy aisle.
Also - if you’re on insulin and you’re scared of lows? Get a CGM. Like, right now. It’s not a luxury. It’s a lifeline. I used to wake up at 3 a.m. with my heart pounding because I thought I was dying. Now I just check my phone. It’s like having a bodyguard in your pocket.
Nicki Aries
February 7, 2026 AT 18:27Can we just acknowledge that the entire diabetes industry is built on fear? We’re told to ‘manage’ our disease, but no one tells us how to live with it. We’re handed a pill, a pamphlet, and a guilt trip. And then we’re supposed to be grateful because ‘at least it’s not worse.’ But what if it is worse? What if your stomach can’t take metformin? What if your kidneys are already failing? What if you can’t afford the new drugs? What if you’re tired of being a statistic?
There’s no ‘right’ way. There’s only your way. And that’s okay. You’re not failing. You’re just human.
Ed Di Cristofaro
February 9, 2026 AT 13:02Y’all are acting like diabetes is some mysterious curse. Nah. It’s just your body saying ‘you’ve been eating like a trash fire for 15 years.’ Metformin gives you diarrhea? Good. Maybe that’s your gut trying to escape. GLP-1s make you lose weight? Good. Maybe you needed to lose 50 lbs anyway. Stop treating meds like they’re magic. They’re not. They’re bandaids on a bullet wound. The real fix? Stop eating the crap. But hey, at least you’ve got a pill to blame now.
Lilliana Lowe
February 10, 2026 AT 20:30It’s statistically inaccurate to claim that ‘most people’ adjust to metformin within a few weeks. The JAMA study cited a 26% incidence of nausea - not ‘most.’ Additionally, the extended-release formulation reduces GI distress by approximately 48%, not ‘half,’ as loosely stated. Furthermore, vitamin B12 deficiency in long-term users is documented at 10–30%, not ‘up to 30%’ - a statistically ambiguous phrase. Precision matters, especially when discussing pharmacokinetics. Also, the term ‘fruity-smelling breath’ is a clinical descriptor of diabetic ketoacidosis, not a casual observation. Please cite sources accurately before disseminating medical information.
Deep Rank
February 12, 2026 AT 09:18Okay so I’ve been on Ozempic for 8 months and I lost 32 pounds and my A1c dropped from 8.9 to 5.6 and I’m so happy but then I started having this weird feeling like my brain is underwater and I can’t think straight and I’m crying at commercials and I don’t know if it’s the drug or if I’m just broken? My mom says I’m dramatic but I think maybe this is what depression feels like? I asked my doctor and she said ‘it’s probably the weight loss’ and I just nodded because I didn’t want to be that person who complains. But I’m scared. Like, really scared. I don’t know if I’m losing weight or losing myself. And I just needed to say it out loud. I’m not okay. And I don’t know what to do. 😔
Bob Cohen
February 12, 2026 AT 22:27That comment from Naomi? Yeah. She’s right. But she’s also the kind of person who thinks ‘I read a study’ means she understands the human experience. The truth? Diabetes isn’t about data. It’s about dignity. It’s about not feeling like a burden. It’s about being able to eat a slice of cake without guilt. It’s about being seen - not just treated. So yeah, the drugs have side effects. So do life, love, and laundry. You don’t quit life because it’s hard. You just learn how to carry it.
Ishmael brown
February 14, 2026 AT 19:26Wait - so SGLT2 inhibitors reduce heart failure hospitalizations by 30%? Cool. But if I get a UTI every other month, am I really ‘protected’? 🤔 Also, why do all these drugs have ‘inhibitor’ in the name? Sounds like a villain from a Marvel movie. ‘Behold, the SGLT2 Inhibitor! It shall drain your sugar… and your dignity!’ 😂 I’m just saying - if your medication makes you feel like a walking science experiment, maybe it’s time to rethink your options. Also - who decided yeast infections were ‘annoying’ and not ‘traumatic’? Just asking.
June Richards
February 16, 2026 AT 05:41Metformin gave me diarrhea for 6 months. I quit. Now I’m on insulin. I gained 15 lbs. I hate it. But at least I don’t have to pee in the middle of the night to avoid a yeast infection. 🤷♀️