DPP-4 Inhibitor Pancreatitis Risk Assessment Tool
This tool helps assess your personal risk of pancreatitis when taking DPP-4 inhibitors based on factors mentioned in the article. This is not medical advice, but a general risk assessment based on published studies.
Your Risk Assessment
When you’re managing type 2 diabetes, finding a medication that lowers blood sugar without causing major side effects is a top priority. DPP-4 inhibitors - also known as gliptins - became popular because they work well, don’t cause weight gain, and rarely lead to low blood sugar. But behind their convenience lies a quiet, serious risk: pancreatitis. It’s rare, but it’s real. And if you’re taking one of these drugs, you need to know the signs - before it’s too late.
What Are DPP-4 Inhibitors?
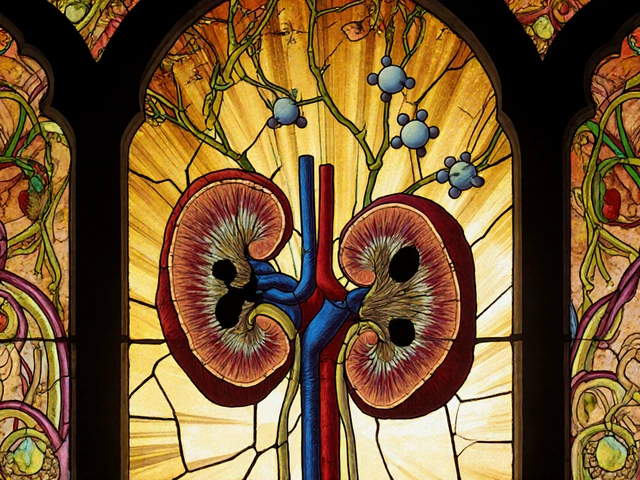
DPP-4 inhibitors are oral diabetes medications that help your body use insulin more effectively. They work by blocking the enzyme DPP-4, which breaks down incretin hormones. Those hormones tell your pancreas to release insulin after meals and reduce the amount of glucose your liver releases. The result? Lower blood sugar - without the crash risk you get with some other drugs.
The first one approved was sitagliptin (Januvia) in 2006. Since then, others followed: saxagliptin (Onglyza), linagliptin (Tradjenta), alogliptin (Nesina), and vildagliptin (not available in the U.S.). Together, they make up about 15% of all oral diabetes prescriptions in the U.S., according to 2022 data. That’s millions of people relying on them daily.
The Pancreatitis Risk: Real, But Rare
The biggest concern with DPP-4 inhibitors isn’t nausea or dizziness - it’s acute pancreatitis. That’s inflammation of the pancreas, often sudden and severe. Symptoms include intense, constant pain in the upper abdomen that can spread to your back, nausea, vomiting, and fever. If ignored, it can lead to organ failure or even death.
Early clinical trials didn’t catch this. Too few people were studied, and pancreatitis is uncommon in healthy adults. But as these drugs were used by millions, reports started piling up. In 2012, the UK’s MHRA confirmed a link. The FDA followed with updated safety labels. By 2019, a meta-analysis of over 47,000 patients showed a 75% higher risk of acute pancreatitis with DPP-4 inhibitors compared to placebo. A 2024 study in Frontiers in Pharmacology found an even stronger signal: a reporting odds ratio of 13.2 - meaning the association isn’t random.
Here’s the key: absolute risk is still low. For every 1,000 people taking a DPP-4 inhibitor for two years, about one to two extra cases of pancreatitis occur. That’s 0.13% extra risk. But if you’re one of them, it’s not a statistic - it’s your life.
Who’s at Higher Risk?
Not everyone faces the same level of danger. Certain factors make pancreatitis more likely:
- History of gallstones or high triglycerides
- Heavy alcohol use
- Previous episodes of pancreatitis
- Obesity
- Smoking
Diabetes itself raises your baseline risk of pancreatitis - so it’s hard to say whether the drug or the disease is to blame. But when both are present, the risk multiplies. A 2023 study tracking 1.2 million patients confirmed that even with diabetes factored in, DPP-4 inhibitors still added a measurable extra risk.

How Do DPP-4 Inhibitors Compare to Other Diabetes Drugs?
It’s not just DPP-4 inhibitors. Other diabetes drugs carry risks too - but not the same ones.
GLP-1 receptor agonists like liraglutide and semaglutide also carry a pancreatitis warning. But their reporting odds ratio is lower than DPP-4 inhibitors - about 9.65 versus 13.2. Still, they’re linked to it.
SGLT2 inhibitors (like empagliflozin and dapagliflozin), on the other hand, have shown significantly lower rates of pancreatitis. In fact, they’re now preferred for patients with heart or kidney disease because they reduce those risks - and they don’t raise pancreatitis risk like DPP-4 inhibitors do.
And here’s something reassuring: multiple studies, including a 2019 meta-analysis of over 55,000 patients, found no increased risk of pancreatic cancer with any of these drugs. That was a big fear early on. It’s not happening.
What Happens If You Get Pancreatitis?
Most cases linked to DPP-4 inhibitors improve after stopping the drug. The MHRA found that in about 82% of reported cases, symptoms resolved once the medication was discontinued. But 17.7% of cases were serious - requiring hospitalization, surgery, or leading to long-term damage.
There’s no test to predict who will get pancreatitis from these drugs. But if you develop new, persistent abdominal pain - especially if it’s severe, lasts more than a few hours, or radiates to your back - don’t wait. Call your doctor. Get blood tests for amylase and lipase (pancreatic enzymes). Get an ultrasound to check for gallstones or swelling.
One case study in Cureus (2021) documented a patient on linagliptin who developed acute pancreatitis after six months. His pain started as mild discomfort, then worsened. He didn’t connect it to his diabetes pill until his doctor asked about medications. He stopped linagliptin immediately. Within days, his pain faded. His enzyme levels returned to normal.

What Should You Do If You’re Taking a DPP-4 Inhibitor?
Don’t panic. Don’t stop cold turkey. But do take action.
- Know the symptoms. Severe, unexplained belly pain. Nausea. Vomiting. Fever. If you feel this way, treat it like an emergency.
- Don’t ignore mild symptoms. Even vague discomfort in your upper abdomen, especially after meals, could be an early sign. Many patients dismiss it as indigestion.
- Ask your doctor about alternatives. If you have risk factors - alcohol use, gallstones, high triglycerides - ask if an SGLT2 inhibitor or GLP-1 agonist might be safer for you.
- Report side effects. If you suspect pancreatitis, report it to your country’s drug safety system (FDA’s MedWatch in the U.S., Yellow Card in the UK). This helps regulators track patterns.
- Get regular checkups. If you’ve been on a DPP-4 inhibitor for over a year, ask your doctor if it’s still the best choice - especially if your A1C is stable.
Why Are These Drugs Still Prescribed?
Because for most people, the benefits still outweigh the risks.
DPP-4 inhibitors don’t cause weight gain. They rarely cause low blood sugar. They’re easy to take - one pill a day. And unlike older drugs like sulfonylureas or insulin, they don’t require constant monitoring or injections.
They also have a clean cardiovascular safety profile. In large trials, they didn’t increase heart attacks or strokes - unlike some earlier diabetes drugs that were pulled from the market. That’s why the American Diabetes Association still lists them as a recommended option in their 2023 Standards of Care.
Global sales for DPP-4 inhibitors hit $5.8 billion in 2022. They’re not going away. But they’re no longer the first choice for many doctors - especially for patients who need heart or kidney protection. That’s where SGLT2 inhibitors and GLP-1 agonists have taken the lead.
The Bottom Line
DPP-4 inhibitors are not dangerous for most people. But they carry a real, documented risk of acute pancreatitis - one that’s rare but serious enough to warrant attention. If you’re on one, you’re not at high risk - but you’re not risk-free.
The goal isn’t to scare you off these drugs. It’s to make sure you’re informed. Know the symptoms. Talk to your doctor. Ask if there’s a better option for you. And if something feels wrong - don’t wait. Pancreatitis gets worse fast. Catching it early can save your life.
Diabetes management is personal. What works for one person might not be right for another. Your health isn’t a one-size-fits-all prescription. It’s a conversation - and you deserve to be part of it.






Adrienne Dagg
December 19, 2025 AT 02:15Glen Arreglo
December 20, 2025 AT 08:03shivam seo
December 22, 2025 AT 02:16benchidelle rivera
December 22, 2025 AT 10:04Andrew Kelly
December 24, 2025 AT 05:28Isabel Rábago
December 25, 2025 AT 15:02Anna Sedervay
December 27, 2025 AT 06:45Mike Rengifo
December 28, 2025 AT 00:03Ashley Bliss
December 28, 2025 AT 05:45Dev Sawner
December 29, 2025 AT 21:07Moses Odumbe
December 31, 2025 AT 19:19