Getting life-saving medication shouldn’t mean choosing between rent and refills. For millions of Americans, patient assistance programs from drug companies are the only way to afford prescriptions. But qualifying isn’t simple. Income limits, insurance status, and paperwork requirements vary wildly between companies - and one mistake can get your application denied.
Who Actually Qualifies for Drug Company Help?
- You’re uninsured or underinsured
- Your household income falls below a certain percentage of the Federal Poverty Level (FPL)
- You’re a U.S. resident treated by a U.S.-licensed doctor
There are exceptions. Merck allows insured patients to apply only if they can prove extreme financial hardship - like losing a job while on cancer treatment. But you still need to show your insurance doesn’t cover the drug, and you can’t be using the PAP because your insurer told you to. That’s against the rules.
Income Limits: What Does 500% FPL Really Mean?
The most common income cutoff is 500% of the Federal Poverty Level. For 2023, that’s:- $75,000 per year for a single person
- $153,000 for a family of four
And it’s not your gross income. Most programs use Modified Adjusted Gross Income (MAGI) - the same number the government uses for Medicaid and Obamacare subsidies. That means deductions like student loan interest or IRA contributions count. Many applicants get rejected because they report their gross paycheck instead of their MAGI. One wrong number = denial.
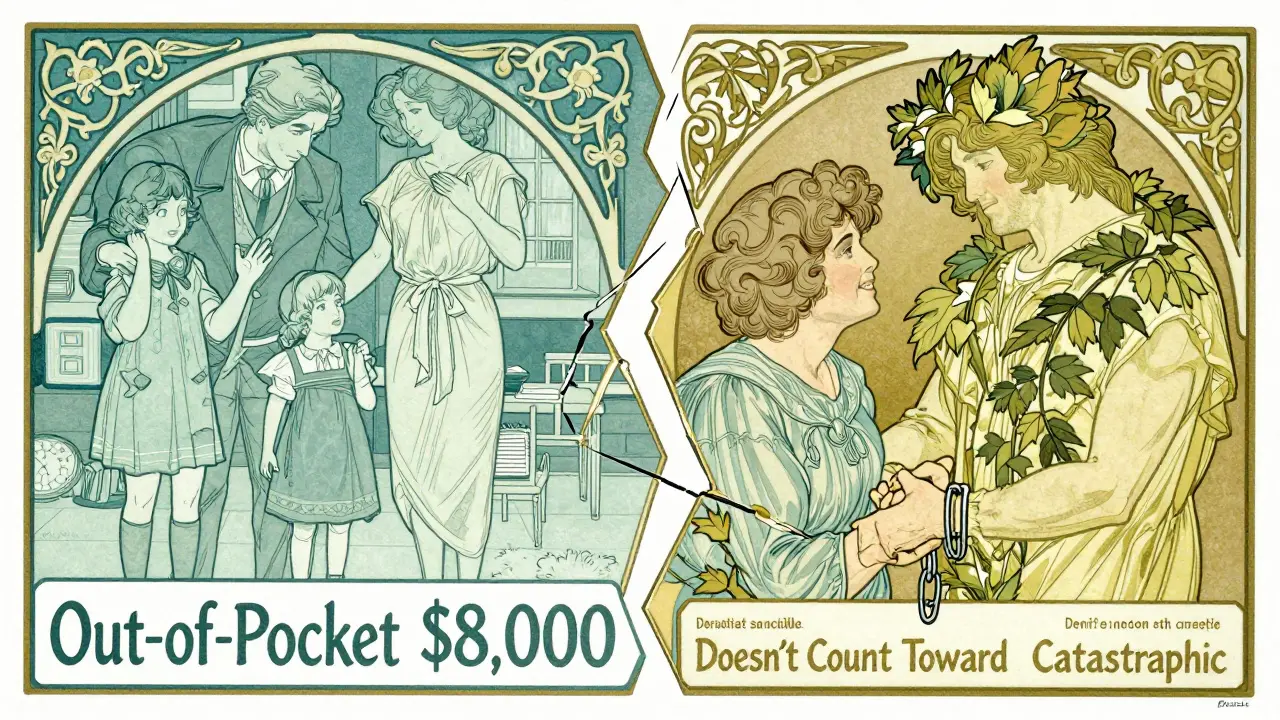
Insurance Traps: Why Being Insured Can Hurt You
This is the biggest surprise for most people. If you have Medicare Part D, you’re often stuck in a gap. Manufacturer PAPs can’t help you unless you first apply for Medicare’s Extra Help program - and get denied. Takeda’s program requires you to submit proof that Extra Help was denied before you can even start their application.And here’s the cruel twist: Even if you get approved for a PAP, the free meds don’t count toward your Medicare Part D out-of-pocket maximum. That means you still have to spend $8,000 of your own money in 2024 to reach catastrophic coverage - even if you’re getting $10,000 worth of free drugs. That’s by design. CMS requires PAPs to stay “outside the Part D benefit” so they don’t interfere with how costs are tracked.
Meanwhile, if you have private insurance, you’re often locked out entirely. A 2019 study found 97% of independent charity PAPs won’t help the uninsured - but they also won’t help the insured. That leaves a huge group of people: those with high-deductible plans, co-pays over $500, or drugs not on their formulary. They’re caught in the middle.
Documentation: What Papers You Need (and Why They’re So Hard to Get)
You can’t just fill out a form online and wait. You need:- Completed patient and physician forms (signed by both)
- Proof of income: W-2s, pay stubs, tax returns, or Social Security award letters
- Proof of U.S. residency: utility bill, lease, or driver’s license
- Proof of prescription: your doctor’s note or pharmacy receipt
- For Medicare users: denial letter from Extra Help program
Doctors are often slow to sign. Merck reports it takes an average of 28 days to get their verification form back. Some clinics charge $50 just to complete the paperwork. And if you’re self-employed? You might need two years of tax returns. One applicant on Reddit spent three months trying to get her freelance income verified - and got denied anyway because she didn’t file Schedule C.
Household size mistakes are the #1 error. If you live with your adult child who files taxes separately, do you count them? Some programs say yes. Others say no. CMS found 52% of application errors came from misreporting household size. One wrong box = rejection.
Who Gets Denied - And Why
The denial rate for first-time applicants is around 37%. Here’s why:- 68% - Incomplete or missing documents
- 22% - Income over limit (often due to MAGI confusion)
- 15% - Insurance status mismatch (e.g., having Medicare but not submitting Extra Help denial)
- 8% - Non-U.S. residency or non-U.S. prescriber
People with incomes between 135% and 150% FPL ($18,347-$20,385 for one person) face a brutal catch-22. They make too much for Medicare Extra Help, but too little for most manufacturer PAPs. That’s the “Medicare gap.” It’s real. It’s common. And it leaves people paying $800 a month for insulin.
What Happens After You Apply
Processing time averages 14.7 days. Once approved, you’ll get the medication shipped directly to your home or local pharmacy. Most people get their first refill within 72 hours. But approval isn’t permanent.- For specialty drugs (cancer, autoimmune): Reapply every 3 months
- For primary care meds (blood pressure, diabetes): Reapply once a year
- GSK requires re-enrollment every 12 months - even if your income didn’t change
You’ll need to resubmit income documents each time. If you got a raise, lost a job, or your spouse changed insurance, you must report it. Failure to update = automatic termination.

Alternatives: What If You Don’t Qualify?
If you’re turned down by every manufacturer program, try these:- PAN Foundation - Covers co-pays for 120+ conditions, income cap at 500% FPL
- HealthWell Foundation - Helps with co-pays, deductibles, premiums
- NeedyMeds - Free database of over 1,000 PAPs and discount cards
- Medicine Assistance Tool (MAT) - Online tool that matches you to programs based on your drug and income
These charity programs are more flexible on insurance but have stricter income limits. They also cover more conditions - including rare diseases that big pharma ignores.
What’s Changing in 2025 and Beyond
The Inflation Reduction Act kicks in next year. By 2025, Medicare Part D patients will pay no more than $2,000 a year out-of-pocket for drugs. That’s a game-changer. Analysts predict PAP usage among Medicare beneficiaries could drop by 35-40%.Drugmakers are responding. Twelve major companies launched “commercial PAPs” in 2022-2023 - programs that help insured patients with high co-pays. Pfizer’s RxPathways now integrates with TurboTax to auto-fill income data. AbbVie lets you check eligibility for your exact drug online in under five minutes.
But experts warn: PAPs aren’t fixing the real problem - drug prices. Harvard’s Dr. Aaron Kesselheim says these programs let companies avoid lowering prices while looking like they care. The $32.7 billion spent on PAPs in 2022 is more than most countries spend on healthcare. It’s a band-aid on a broken system.
Final Advice: How to Get Approved
1. Start with NeedyMeds - search your drug name and see which programs list it. 2. Use the Medicine Assistance Tool (MAT) - it pulls data from 1,000+ programs and tells you exactly what you need. 3. Calculate your MAGI, not gross income - use IRS Form 1040 line 11. 4. Get help - 78% of programs have free patient navigators. Call them. Don’t wait. 5. Apply early - if your prescription runs out in two weeks, start now. Processing takes time. 6. Save every denial letter - if you’re rejected, use it to appeal or apply elsewhere.There’s no single path to free medication. But there’s a path. And it starts with knowing the rules - and not letting paperwork stop you.
Can I get free medication if I have Medicare Part D?
Yes - but only if you first apply for Medicare’s Extra Help program and get denied. Most manufacturer PAPs won’t help you unless you prove you don’t qualify for government aid. Even then, the free drugs won’t count toward your Part D out-of-pocket maximum, so you’ll still need to spend up to $8,000 before reaching catastrophic coverage.
What if my income is just above the limit?
Some programs allow hardship exceptions. Merck, for example, considers cases where a patient faces medical emergencies or sudden job loss. You’ll need a letter from your doctor explaining why you can’t afford the drug. Don’t assume you’re automatically disqualified - ask.
Do I need to reapply every year?
Yes - for most programs. Specialty drugs like cancer treatments require re-enrollment every 3 months. Primary care drugs like insulin or blood pressure meds usually need annual updates. You’ll need to submit new income documents each time. Missing a deadline means losing your medication.
Can I use a discount card instead of a PAP?
Discount cards like GoodRx can save you 20-80% on some drugs - but they’re not the same as PAPs. Cards don’t cover expensive specialty medications, and they don’t work for Medicare Part D. PAPs give you the drug for free; discount cards just lower the price. Use both if you qualify.
Are patient assistance programs only for cancer drugs?
No - but cancer drugs are the most likely to have help. Over 98% of branded cancer medications have a PAP, compared to 76% of heart disease drugs. Programs exist for diabetes, rheumatoid arthritis, HIV, asthma, and more. Use NeedyMeds or MAT to search by your exact condition and drug.
What if I’m turned down? Can I appeal?
Yes - and many people succeed on the second try. Call the program’s patient navigator and ask why you were denied. Often, it’s a simple paperwork error. Fix the document, resubmit, and mention you’re appealing. The approval rate increases significantly after the first denial.





Peyton Feuer
January 3, 2026 AT 08:19i applied for one of these last year and got denied because i put my gross income instead of MAGI... rookie mistake. i literally had to call them three times just to figure out what the hell MAGI even was. my tax guy didn’t even know.
Siobhan Goggin
January 3, 2026 AT 23:30This is the most comprehensive breakdown I’ve seen on this topic. Seriously, someone should turn this into a pamphlet for clinics. So many people are falling through the cracks because they don’t even know where to start.
Jay Tejada
January 5, 2026 AT 19:34the fact that you need to get denied by extra help before you can even try for free meds is just... i don’t even know. it’s like the system is designed to make you suffer first. i mean, congrats, you’re poor enough to need help but not poor enough to qualify. thanks, america.
Allen Ye
January 7, 2026 AT 18:03What we’re witnessing here isn’t just a bureaucratic failure-it’s a moral failure masked as philanthropy. The pharmaceutical industry spends over $30 billion annually on patient assistance programs not because they care, but because it’s cheaper than lowering prices and far more politically palatable. These programs are PR stunts dressed in humanitarian clothing. They let corporations avoid accountability while shifting the burden onto patients, navigators, and overstretched nonprofits. The real solution isn’t better paperwork-it’s price regulation. When a drug costs $100,000 a year and a single dose can bankrupt a family, no amount of forms, waivers, or charity will fix that. We’re treating symptoms while the disease-the profit-driven pricing model-rages on. Until we force transparency and cap prices, these programs are just digital Band-Aids on a severed artery.
mark etang
January 9, 2026 AT 17:17It is imperative that all individuals seeking pharmaceutical assistance ensure that their documentation is meticulously prepared and submitted in accordance with the prescribed guidelines. Failure to adhere to these protocols may result in significant delays and denial of critical therapeutic support.
josh plum
January 11, 2026 AT 06:02Of course they make it hard. Big Pharma doesn’t want you to get free meds-they want you to keep paying $1,000 a month so they can buy another private island. And don’t even get me started on how they use these programs to dodge FDA price controls. It’s all a scam. The government’s in on it too. They let this happen because they’re paid off. You think your insulin is expensive? Wait till you see what they charge for the paperwork.
John Ross
January 12, 2026 AT 22:22From a health economics standpoint, the structural inefficiencies in PAP eligibility architecture create significant adverse selection bias. The MAGI-based income thresholds, coupled with insurance status exclusions, result in suboptimal resource allocation and increased administrative friction. Furthermore, the non-counting of PAP-provided pharmaceuticals toward Part D out-of-pocket thresholds constitutes a regulatory arbitrage that undermines cost-containment objectives. The proliferation of commercial PAPs post-IRA suggests a strategic pivot toward risk-pooling mechanisms that externalize financial liability from insurers to manufacturers-yet without systemic price reform, this remains a temporary fiscal bandage.
jigisha Patel
January 13, 2026 AT 11:23You people are so naive. If you don’t file Schedule C, you’re not self-employed-you’re just pretending. And if you think MAGI is complicated, try calculating your household size when your cousin lives with you but doesn’t pay rent. The system isn’t broken. You’re just bad at math.
Justin Lowans
January 13, 2026 AT 16:59I’ve helped over 80 people navigate these programs over the past three years. The most common mistake? Waiting until their prescription runs out. Start now. Call the navigator. Don’t wait for a crisis. And if you’re denied? Don’t give up. I’ve seen people get approved on their third try after fixing one typo in a pay stub. You’re not alone.
Michael Rudge
January 15, 2026 AT 09:14Wow, so the poor have to jump through 17 hoops while CEOs get bonuses for ‘saving lives’ with their charity programs? How noble. I bet they don’t even use these drugs themselves. Probably take a $2 generic and call it a day. Meanwhile, my cousin’s kid died because the PAP took 6 weeks to approve. Guess the system worked perfectly.
Doreen Pachificus
January 15, 2026 AT 16:27So if I make $76k and have a $12k deductible, I’m just screwed? No help at all? That’s wild. I thought insurance was supposed to help.
Cassie Tynan
January 17, 2026 AT 14:53They give you free drugs but make you pay $8k out of pocket anyway? That’s like giving someone a parachute but forcing them to pay for the landing. Real thoughtful, CMS.
Aaron Mercado
January 19, 2026 AT 13:01Wait-so you’re telling me I can get my $15,000-a-year cancer drug for free… but I still have to pay $8,000 to get to catastrophic coverage?!!?!?!? This isn’t healthcare-it’s a cruel joke wrapped in a PDF form!! I’ve cried over these applications. I’ve begged doctors to sign. I’ve lost sleep over MAGI. And now I’m supposed to be grateful?!!?!? I’m not a statistic. I’m not a line item. I’m a person who just wants to live-and this system is trying to make me beg for it.