Psychiatric Medication Interaction Checker
Check Your Medications
Interaction Result
Why Mixing Psychiatric Drugs Can Be Life-Threatening
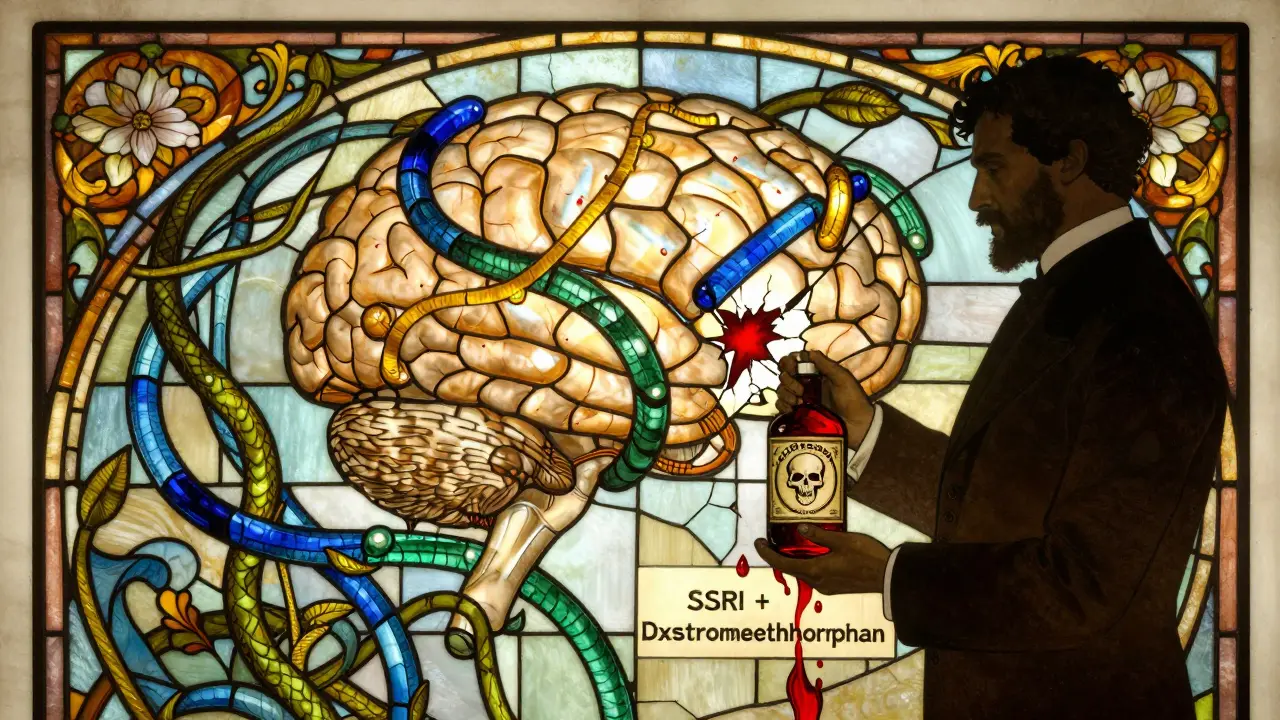
It’s not uncommon for someone with depression to also struggle with anxiety. Or for bipolar disorder to come with insomnia and psychosis. That’s why many people end up on more than one psychiatric medication. But mixing these drugs isn’t like combining vitamins. One wrong combo can trigger serotonin syndrome - a condition that can kill you in hours.
Back in 2023, a 42-year-old man in Bristol was admitted to the ER after taking his usual antidepressant and a new over-the-counter cold remedy. He had a fever of 104°F, muscle rigidity, and confusion. He didn’t know the cold medicine contained dextromethorphan - a serotonin booster. Within 48 hours, he was in intensive care. This isn’t rare. Around 30 to 50% of serious adverse events in psychiatric care come from drug interactions, according to the American Association of Psychiatric Pharmacists.
The Three Neurotransmitters That Rule Your Brain
Psychiatric drugs work by changing how your brain handles three key chemicals: serotonin, norepinephrine, and dopamine. Each class of medication affects them differently.
SSRIs like fluoxetine and sertraline boost serotonin. That’s good for mood, but too much serotonin = danger. SNRIs like venlafaxine raise both serotonin and norepinephrine - which helps with energy and focus, but also raises blood pressure. TCAs like amitriptyline hit serotonin and norepinephrine too, but they also block acetylcholine, causing dry mouth, constipation, and heart rhythm problems. Antipsychotics like risperidone and quetiapine block dopamine - which calms hallucinations, but can make you move like a robot. And then there are MAO inhibitors like phenelzine - the most dangerous class. They prevent your body from breaking down serotonin, norepinephrine, and dopamine at all. One slip-up with another drug, and your brain gets flooded.
MAO Inhibitors: The Most Dangerous Class
If you’re on an MAO inhibitor - like phenelzine (Nardil) or tranylcypromine (Parnate) - you can’t take almost any other psychiatric drug without risking death. Combining MAOIs with SSRIs, SNRIs, or even some painkillers like tramadol can trigger serotonin syndrome. Symptoms start fast: shivering, sweating, rapid heartbeat, high blood pressure, then muscle stiffness, seizures, and organ failure.
Doctors won’t prescribe MAOIs unless everything else has failed. And if you switch off them, you must wait at least two weeks before starting an SSRI. That’s not a suggestion - it’s a rule. One study found that 12% of patients who skipped the washout period ended up in the hospital. And it’s not just drugs. Foods like aged cheese, cured meats, and tap beer can also trigger reactions if you’re on an MAOI. The Black Book of Psychotropic Dosing and Monitoring calls this the most preventable cause of psychiatric drug deaths.
SSRIs and the Silent Killer: Serotonin Syndrome
You don’t need an MAOI to get serotonin syndrome. It happens with SSRIs too - especially when stacked with other serotonin boosters. Common culprits include:
- Tramadol (a painkiller)
- Dextromethorphan (in cough syrups)
- Triptans (for migraines)
- St. John’s Wort (herbal supplement)
- MDMA (ecstasy)
Fluvoxamine is the worst offender among SSRIs because it blocks the liver enzyme CYP1A2, which breaks down many other drugs. That means if you’re on fluvoxamine and take clozapine, the clozapine builds up to toxic levels. Sertraline and citalopram are safer choices if you’re on multiple meds - they don’t interfere with liver enzymes as much.
Signs of serotonin syndrome come on fast - usually within hours. Mild cases feel like the flu: nausea, tremors, restlessness. Severe cases? High fever, seizures, unconsciousness. Mortality hits 2 to 12% if not treated immediately. There’s no test for it. Diagnosis is based on symptoms and recent drug use. If you’re on an SSRI and start feeling worse after adding something new - get help right away.
TCAs: Old but Deadly
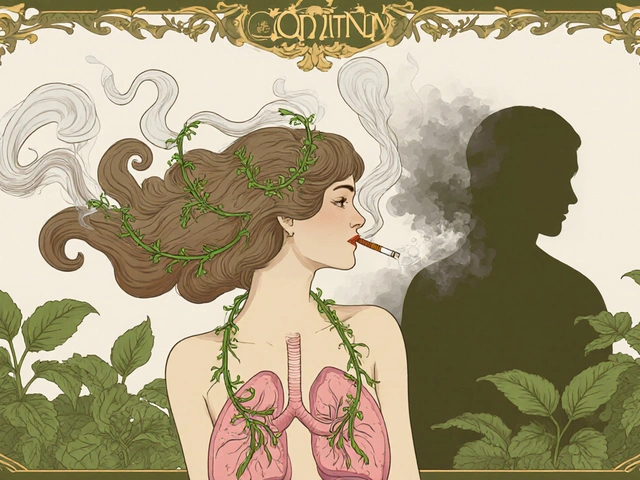
Tricyclic antidepressants like amitriptyline and nortriptyline are rarely first-line anymore - and for good reason. They’re anticholinergic, meaning they dry out your mouth, blur your vision, and slow your gut. But worse, they can mess with your heart rhythm. When combined with other anticholinergic drugs - like diphenhydramine (Benadryl), some antipsychotics, or even bladder medications - the risk of dangerous arrhythmias spikes.
And if you drink alcohol while on a TCA? You’re adding fuel to the fire. Both depress your central nervous system. The result? Extreme drowsiness, poor coordination, even respiratory failure. The Black Book warns that TCA-alcohol combos are a leading cause of accidental overdose in older adults. Even small amounts of alcohol can be risky.
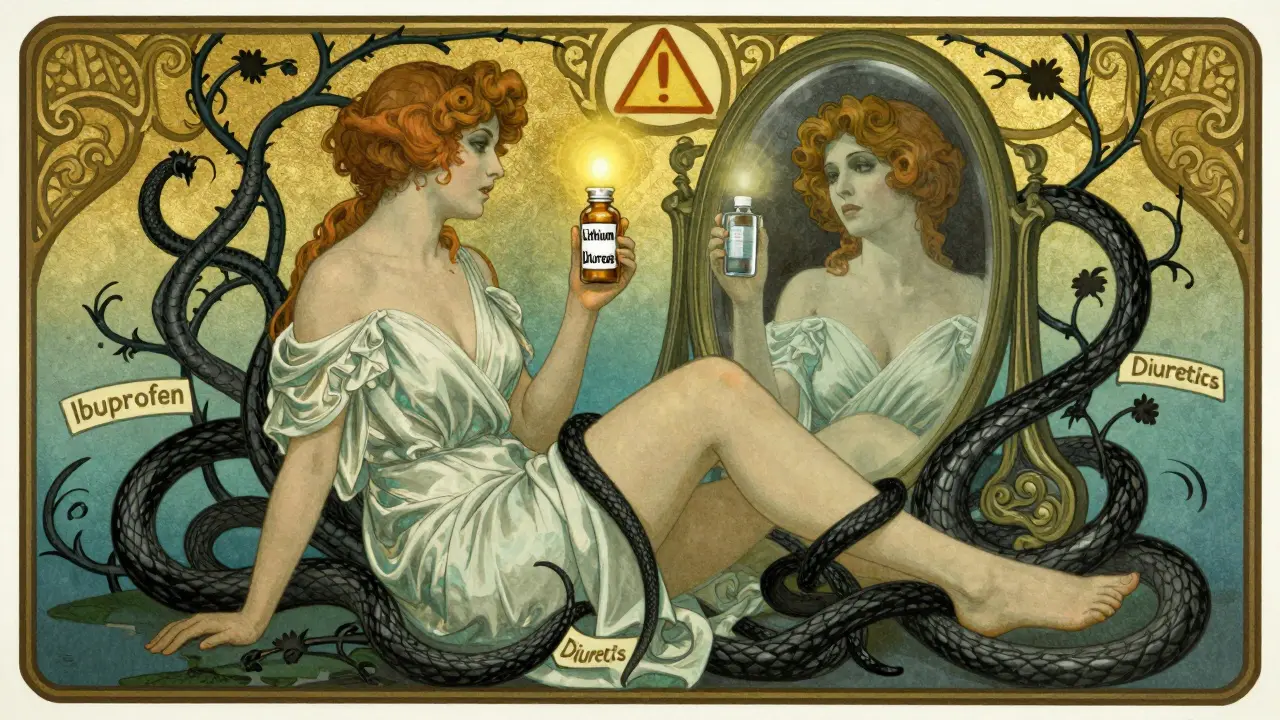
Lithium: A Tiny Window Between Help and Harm
Lithium is one of the oldest and most effective mood stabilizers for bipolar disorder. But it has a razor-thin safety margin. The therapeutic range is 0.6 to 1.0 mmol/L. Go over 1.2, and you’re in danger. Over 1.5, and you risk coma or death.
Many common drugs can push lithium levels up - especially NSAIDs like ibuprofen and naproxen. They reduce kidney blood flow, so lithium doesn’t get flushed out. One study showed NSAIDs can spike lithium levels by 25 to 50%. Even diuretics (water pills) and ACE inhibitors can do it. That’s why anyone on lithium needs regular blood tests - every 3 months if stable, every 2 weeks after starting a new drug.
Dehydration makes it worse. A hot day, a bad stomach bug, or skipping water can turn a safe dose into a toxic one. Patients are told: drink water, avoid NSAIDs, and call your doctor if you feel shaky, nauseous, or confused.
Antipsychotics and the Hidden Risks
Not all antipsychotics are the same. Quetiapine has low interaction risk. Risperidone and olanzapine can cause weight gain and high blood sugar. But clozapine? It’s powerful for treatment-resistant schizophrenia - but it can wipe out your white blood cells. That’s called agranulocytosis. It’s rare, but deadly. So patients on clozapine need weekly blood tests for the first six months.
Also, many antipsychotics slow your heart rhythm. Combine them with SSRIs like fluoxetine or fluvoxamine - which block the same liver enzymes - and your QT interval can stretch dangerously. That can lead to torsades de pointes, a heart rhythm that can kill. Always get an ECG before starting, and again after a few weeks.
What You Can Do to Stay Safe
Here’s what actually works in real life:
- Know your meds. Write down every pill you take - including supplements and OTC drugs. Bring this list to every appointment.
- Ask about interactions. Don’t assume your doctor knows. Say: “Is this safe with my other meds?”
- Watch for red flags. New fever, confusion, muscle rigidity, rapid heartbeat, or sudden agitation? Call 999. Don’t wait.
- Use a pharmacy that tracks interactions. Many UK pharmacies now flag dangerous combos when you pick up prescriptions. Use them.
- Never start or stop a psychiatric drug without talking to your prescriber. Even small changes can trigger reactions.
The Future: Personalized Medicine Is Here
Genetic testing is changing the game. Some people have a CYP2D6 or CYP2C19 gene variant that makes them slow metabolizers. That means standard doses of antidepressants build up to toxic levels. The Clinical Pharmacogenetics Implementation Consortium (CPIC) now has clear guidelines for testing these genes before prescribing.
Some clinics in the UK are already using digital tools that scan your entire medication list in real time. One trial showed a 37% drop in dangerous interactions when these systems were used with clinician training. AI models are being tested now - they’ll soon predict your personal risk based on your genes, age, liver function, and current meds.
Final Reality Check
Psychiatric meds save lives. But they’re not harmless. The biggest risk isn’t the drugs themselves - it’s the assumption that combining them is safe. The truth? Many people are on three, four, or five psychiatric drugs. And most don’t know the risks.
Don’t be one of them. Learn your meds. Ask questions. Track your symptoms. And if something feels wrong - trust your gut. It could save your life.
Can I take ibuprofen with lithium?
No, not without close monitoring. Ibuprofen and other NSAIDs can reduce kidney function, causing lithium to build up in your blood. This can push levels from safe (0.8 mmol/L) into toxic range (over 1.2 mmol/L). If you need pain relief, talk to your doctor about alternatives like paracetamol. If you must use ibuprofen, get a blood test within 5 days and watch for symptoms like tremors, nausea, or confusion.
Is it safe to mix SSRIs with St. John’s Wort?
Absolutely not. St. John’s Wort increases serotonin in the brain, just like SSRIs. Combining them raises your risk of serotonin syndrome - a potentially fatal condition. Even if you’ve taken St. John’s Wort for months, adding an SSRI can trigger a reaction. There’s no safe dose of this combo. Stop the herb before starting an SSRI, and wait at least two weeks.
Why are MAO inhibitors so dangerous with other antidepressants?
MAO inhibitors stop your body from breaking down serotonin, norepinephrine, and dopamine. When you add another drug that boosts serotonin - like an SSRI or SNRI - your brain gets flooded. This causes serotonin syndrome: high fever, muscle rigidity, seizures, and organ failure. The risk is so high that doctors require a two-week washout period between stopping an MAOI and starting any other antidepressant. Skipping this step has killed people.
Can I drink alcohol while on psychiatric meds?
It depends. With SSRIs or SNRIs, a small amount might be okay - but it can worsen drowsiness and depression. With TCAs or benzodiazepines, even one drink can cause dangerous sedation or breathing problems. With MAOIs, alcohol can trigger a hypertensive crisis. The safest answer? Avoid alcohol entirely unless your doctor says otherwise. Many psychiatric meds already affect your liver, and alcohol adds stress. Don’t gamble with your brain.
What should I do if I accidentally take a dangerous combo?
Call 999 immediately. Don’t wait for symptoms. If you took an SSRI with tramadol or an MAOI with another antidepressant, you could be in danger even if you feel fine. Tell emergency staff exactly what you took and when. Bring your pill bottles. Early treatment - like giving benzodiazepines or cyproheptadine - can stop serotonin syndrome before it kills you. Seconds matter.
How often should I get blood tests on psychiatric meds?
It varies. Lithium: every 3 months, or sooner after starting a new drug. Clozapine: weekly for the first 6 months, then monthly. Anticonvulsants like valproate: liver tests every 3 months. If you’re on multiple meds or have kidney/liver issues, your doctor may test more often. Always follow your monitoring schedule - skipping tests is how people end up in the hospital.