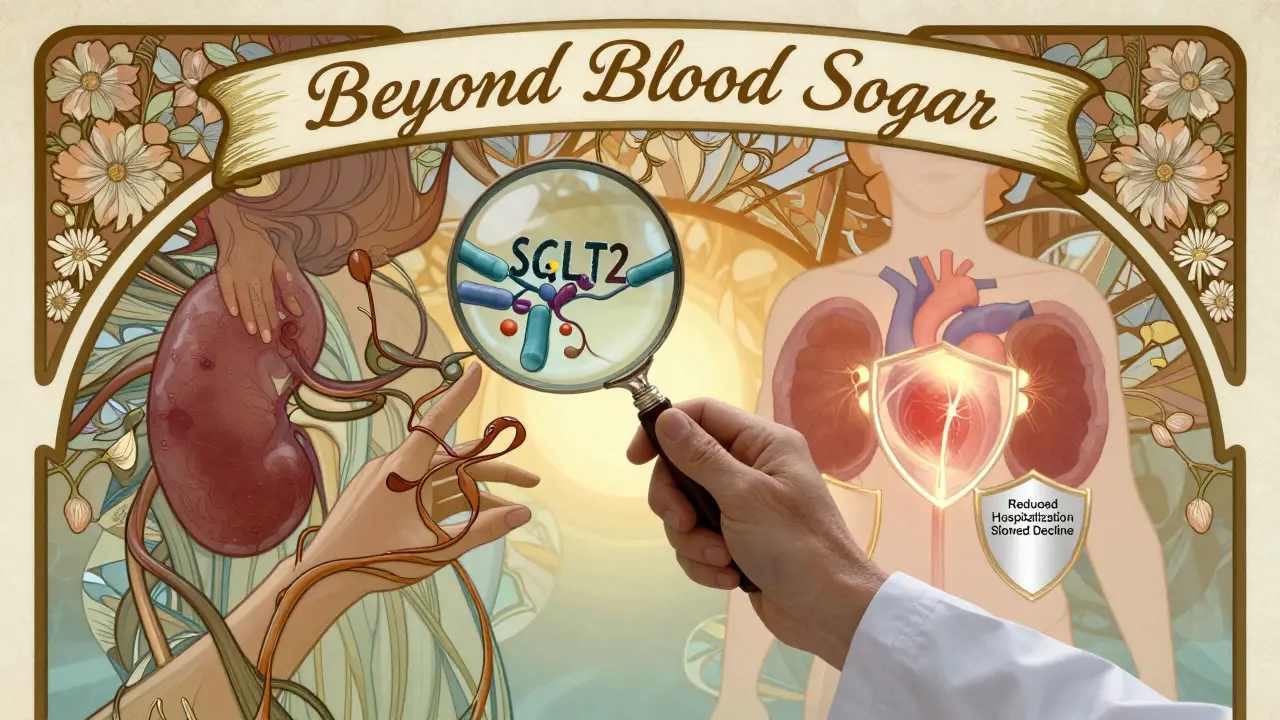
For years, treating type 2 diabetes meant one thing: lower blood sugar. But today, the goal has changed. It’s not just about HbA1c numbers anymore. Doctors now look at whether a medication protects the heart and kidneys - because for many people with diabetes, those are the real threats. SGLT2 inhibitors are at the center of this shift. These aren’t just another pill to control glucose. They’re changing how we treat diabetes - and saving lives in the process.
How SGLT2 Inhibitors Actually Work
Unlike metformin or insulin, SGLT2 inhibitors don’t rely on the pancreas or insulin sensitivity. They work in the kidneys. Specifically, they block a protein called SGLT2, which normally reabsorbs glucose from urine back into the bloodstream. When this protein is turned off, excess sugar leaves the body through urine - no insulin needed.
This simple trick lowers blood sugar by about 0.5% to 1.0% on average. But here’s the surprise: it also causes a small drop in blood pressure and leads to modest weight loss - around 2 to 3 kilograms over a few months. That’s because you’re losing not just sugar, but also water and sodium. The body flushes out about 70 to 100 grams of glucose a day. That’s roughly 280 to 400 extra calories lost daily.
The drugs in this class - empagliflozin (Jardiance), dapagliflozin (Farxiga), canagliflozin (Invokana), and ertugliflozin (Steglatro) - all work the same way. They’re taken once a day, orally. No injections. No complex dosing. Just a pill that helps your kidneys do something they’re already designed to do: filter waste.
Heart Protection You Can’t Ignore
The real breakthrough came in 2015, with the EMPA-REG OUTCOME trial. Researchers gave empagliflozin to over 7,000 people with type 2 diabetes and known heart disease. After three years, those taking the drug had a 38% lower risk of dying from heart-related causes. That’s not a small number. It’s one of the biggest drops ever seen in a diabetes drug trial.
Other trials confirmed it. The CANVAS Program showed canagliflozin cut major heart events - like heart attacks and strokes - by 14%. DECLARE-TIMI 58 found dapagliflozin reduced hospitalizations for heart failure by 17%. These weren’t just side effects. They were consistent, repeatable, and powerful.
Even more surprising? These drugs help people with heart failure - even if they don’t have diabetes. The DAPA-HF and EMPEROR-Reduced trials proved dapagliflozin and empagliflozin reduced hospitalizations and death in heart failure patients regardless of blood sugar levels. That’s why the American Heart Association now recommends SGLT2 inhibitors for all heart failure patients with reduced pumping ability, whether they have diabetes or not.
Kidney Benefits That Are Groundbreaking
Diabetic kidney disease is one of the leading causes of dialysis in the U.S. And until recently, few drugs could slow it down. That changed with the CREDENCE trial in 2019. Canagliflozin was tested in over 4,400 people with type 2 diabetes and early kidney damage. After 2.6 years, those on the drug had a 30% lower risk of kidney failure, doubling of creatinine, or death from kidney disease.
The EMPA-KIDNEY trial in 2023 took it even further. Empagliflozin reduced major kidney events by 28% in people with chronic kidney disease - even if they didn’t have diabetes. This is huge. It means these drugs might soon be used to protect kidneys in a much broader group of patients, not just those with high blood sugar.
Doctors used to worry when they saw a small dip in kidney function after starting an SGLT2 inhibitor. But now we know: that’s not damage. It’s a sign the drug is working. The pressure inside the kidney’s filtering units drops, which reduces long-term strain. The eGFR usually stabilizes after 2 to 3 months. This isn’t kidney injury - it’s kidney protection.
How They Compare to Other Diabetes Drugs
Metformin is still the first choice for most people with type 2 diabetes. It’s cheap, safe, and helps with weight. But it doesn’t reduce heart attacks or kidney failure the way SGLT2 inhibitors do. Sulfonylureas like glipizide can cause dangerous low blood sugar and weight gain. DPP-4 inhibitors like sitagliptin are neutral on weight and heart risk, but offer no kidney protection.
Here’s a quick comparison:
| Medication | HbA1c Reduction | Heart Risk Reduction | Kidney Protection | Weight Change | Cost (Monthly, US) |
|---|---|---|---|---|---|
| SGLT2 Inhibitors | 0.5-1.0% | Up to 38% lower cardiovascular death | Yes - proven in multiple trials | Loss of 2-3 kg | $520-$600 |
| Metformin | 0.5-1.5% | No proven benefit | No proven benefit | Neutral | $4-$10 |
| Sulfonylureas | 1.0-1.5% | No benefit | No benefit | Gain of 1-3 kg | $10-$15 |
| DPP-4 Inhibitors | 0.5-0.8% | Neutral | No benefit | Neutral | $350-$400 |
The cost of SGLT2 inhibitors is a real concern. Generic versions aren’t available in the U.S. yet, but they’re expected to arrive between 2025 and 2028. Until then, insurance coverage varies widely. Many patients report struggles with prior authorizations or high copays.
What You Need to Watch Out For
No drug is perfect. SGLT2 inhibitors have risks. The most common side effect is genital yeast infections - about 4% to 5% of users, compared to 1% on placebo. These are treatable, but annoying. Urinating more often is also common, especially at first.
The bigger concern is diabetic ketoacidosis (DKA). It’s rare - only about 0.1% to 0.3% of users - but it can happen even when blood sugar isn’t very high. This is called euglycemic DKA. It’s dangerous because it doesn’t trigger the usual warning signs. If you’re sick, fasting, or having surgery, your doctor may tell you to stop the drug temporarily.
Canagliflozin has a small increased risk of lower-limb amputations - about 6.3 events per 1,000 patient-years compared to 3.4 on placebo. That’s why doctors avoid it in people with poor circulation, foot ulcers, or a history of amputation.
These drugs aren’t for everyone. They’re not approved for type 1 diabetes. And they shouldn’t be used if your kidney function is too low - eGFR below 30. Dose adjustments are needed if your eGFR is below 60.
Real Stories, Real Impact
On diabetes forums, people share what it’s really like:
- One man on Reddit lost 12 pounds in three months and said his energy improved - but he hated the constant need to pee.
- A woman on PatientsLikeMe saw her heart’s pumping ability improve from 25% to 35% after adding Farxiga to her treatment. Her cardiologist called it "remarkable."
- Another user had two yeast infections in six months and had to switch drugs.
These aren’t outliers. They’re common experiences. The trade-off is often worth it: better heart function, slower kidney decline, and weight loss - for a few extra doctor visits and a higher pill cost.
What’s Next for SGLT2 Inhibitors?
The science is still evolving. The DELIVER trial showed dapagliflozin helps people with heart failure and preserved ejection fraction - a type of heart failure that’s been hard to treat. The American Diabetes Association is expected to update its guidelines in early 2024 to include SGLT2 inhibitors for prediabetes and metabolic syndrome.
Researchers are now asking: Why do these drugs work so well? Is it the sugar loss? The blood pressure drop? Or something else - like increased ketones, which may act as a cleaner fuel for the heart and kidneys? Early data from the SUGAR-DM trial suggests ketones might be part of the answer.
By 2025, SGLT2 inhibitors could be prescribed to nearly half of all heart failure patients in the U.S. And once generics arrive, prices could drop by 60% to 70%. That will make them accessible to millions more.
For patients with type 2 diabetes - especially those with heart or kidney problems - SGLT2 inhibitors are no longer optional. They’re part of the standard of care. The goal isn’t just to control blood sugar anymore. It’s to keep you alive, active, and out of the hospital.
Are SGLT2 inhibitors safe for people with kidney disease?
Yes - but only if kidney function isn’t too low. Most SGLT2 inhibitors can be used when eGFR is above 30 mL/min/1.73m². Some, like dapagliflozin and empagliflozin, are even approved for use in chronic kidney disease without diabetes. The key is monitoring. An initial drop in eGFR is normal and expected - it’s not damage, it’s protection. Your doctor will check your kidney function before starting and again after 3 months.
Do SGLT2 inhibitors cause low blood sugar?
Not usually - unless you’re also taking insulin or sulfonylureas. Because SGLT2 inhibitors work independently of insulin, they rarely cause hypoglycemia on their own. That’s one reason they’re safer than older drugs like glipizide or glyburide. But if you’re on multiple medications, your doctor may need to adjust your other doses to avoid low blood sugar.
Can I stop taking SGLT2 inhibitors if my blood sugar improves?
Don’t stop without talking to your doctor. Even if your HbA1c drops to 6.0%, the heart and kidney benefits continue. Stopping the drug means losing that protection. These drugs work best when taken long-term. The goal isn’t just to get your sugar down - it’s to keep your organs healthy for years to come.
Why do I need to drink more water on SGLT2 inhibitors?
Because you’re losing more fluid through urine. The drug causes osmotic diuresis - meaning your body pulls water out along with glucose. That can lead to dehydration, especially in older adults or during hot weather. Drink water regularly, especially if you’re exercising or sick. Avoid alcohol and caffeine in excess, as they can make dehydration worse.
What should I do if I get sick or need surgery?
Call your doctor. During illness, fasting, or surgery, your risk of diabetic ketoacidosis (DKA) increases - even if your blood sugar isn’t high. Your provider may tell you to pause the SGLT2 inhibitor for a few days. Don’t stop it on your own. Follow your doctor’s plan. Resume only when you’re eating normally again and feeling well.






Pavan Vora
January 6, 2026 AT 05:32So these pills make you pee out sugar?? In India, we call this "natural diuretic effect"... but honestly, if my uncle with diabetes can lose weight and not die of heart attack, i'll take the frequent bathroom breaks. My aunt on Jardiance lost 11kg in 6 months, no gym, just pills and chai. Also, yeast infections? Yeah, we know that one. Coconut oil helps. No joke.
Ryan Barr
January 8, 2026 AT 03:15Empagliflozin saved my life. No fluff. Just facts.
Dana Termini
January 9, 2026 AT 18:40I’ve been on Farxiga for two years now. My eGFR dipped at first, scared me to death. But my nephrologist explained it was protective - not damage. Now my numbers are stable, and my heart function improved. It’s not magic, but it’s science that actually works. I wish more people knew this.
Wesley Pereira
January 10, 2026 AT 06:04Let’s be real - metformin’s the OG, but SGLT2i are the MVPs now. You’re telling me a $600/month pill reduces CV death by 38%? And you’re shocked? The FDA’s behind this. The AHA’s behind this. Even Big Pharma’s scrambling to copy it. Meanwhile, my cousin’s on glipizide and still eating donuts. Good luck with that.
Also, euglycemic DKA? Yeah, it’s rare, but if you’re keto-ing or fasting for Ramadan? Stop the drug. Don’t be that guy.
Isaac Jules
January 10, 2026 AT 14:44Oh wow, another "miracle drug" from Big Pharma. Let me guess - side effects are "manageable" and "rare"? 4-5% yeast infections? That’s not rare, that’s a nuisance epidemic. And amputations? 6.3 per 1000? That’s a damn red flag. You’re glorifying a drug that makes you pee sugar while your toes fall off. Congrats.
And the cost? $600/month? For a pill that does what metformin does - but worse? You’re selling snake oil with a fancy trial name.
Amy Le
January 11, 2026 AT 15:18Of course SGLT2 inhibitors work - they’re just fancy diuretics with a marketing team. America spends billions on drugs that make you pee more. Meanwhile, in China, they use herbs and acupuncture. We’re so obsessed with pills we forget the body heals itself. Also, why are we giving these to non-diabetics? Next they’ll prescribe them for weight loss. 🤦♀️
Joann Absi
January 13, 2026 AT 13:47MY UNCLE GOT HIS LEG AMPUTATED ON CANAGLIFFLOZIN. I’M NOT KIDDING. HE WAS 52. HE HAD A SMALL CUTO ON HIS TOE. DOCTORS SAID "IT’S JUST A SIDE EFFECT." NOW HE’S IN A WHEELCHAIR. 🤬 THIS ISN’T MEDICINE - IT’S A GAME OF RUSSIAN ROULETTE WITH YOUR BODY. 🇺🇸💊💀
Jeane Hendrix
January 13, 2026 AT 19:14I’ve been on dapagliflozin for 18 months. My HbA1c went from 8.2 to 6.1. I lost 7 lbs. My heart failure symptoms improved - less swelling, less fatigue. The only downside? Constant peeing. Like, 8x a day. But honestly? Worth it. I’d rather pee than be on a ventilator. Also, my doc said the initial eGFR dip is normal - it’s the kidneys relaxing, not failing. Learned that the hard way.
And yes, yeast infections suck. But over-the-counter fluconazole fixes it. Don’t panic. Just talk to your provider.
Rachel Wermager
January 15, 2026 AT 08:52Actually, the mechanism isn’t just osmotic diuresis - it’s the reduction in intraglomerular pressure via tubuloglomerular feedback. That’s why renal protection occurs independently of glycemic control. Also, the ketone hypothesis is gaining traction - β-hydroxybutyrate acts as a more efficient cardiac fuel and reduces oxidative stress in renal tubules. SUGAR-DM data suggests a 22% increase in circulating ketones within 72 hours of initiation. This isn’t just a glucose-lowering agent - it’s a metabolic modulator.
Leonard Shit
January 15, 2026 AT 21:11My grandma’s on Jardiance. She’s 78, diabetic, heart failure. She says she feels "lighter." Not in a spiritual way - like, physically. Less puffiness. And she’s not peeing every 20 minutes anymore - just the first week. She’s also not in the hospital anymore. So yeah, I’ll take the $600/month. Even if it’s a little expensive, it’s cheaper than a stent.
Also, the yeast thing? She uses cotton underwear and wipes after peeing. Boom. Problem solved. No drama.
Brian Anaz
January 17, 2026 AT 13:29These drugs are great. But why are we letting insurance companies decide who gets them? My friend got denied 3 times. He’s got CKD and heart disease. He’s on disability. He can’t afford $600. This isn’t healthcare - it’s a luxury for the rich. Fix the system before you praise the pill.
Venkataramanan Viswanathan
January 19, 2026 AT 10:27In India, we have no access to these drugs. They cost more than my monthly salary. My father has diabetes and kidney disease. He takes metformin and amlodipine. He survives. But I wonder - if he had Farxiga, would he still be here? I don’t know. But I know this: science is not equal. Some get miracles. Others get prayers.