Lithium-NSAID Interaction Calculator
Lithium Levels & NSAID Interaction Risk
Enter your current lithium level and select the NSAID you're taking to estimate the risk of toxicity. Remember: even occasional NSAID use can be dangerous with lithium.
Every year, thousands of people on lithium for bipolar disorder take ibuprofen or naproxen for a headache, back pain, or arthritis flare-up-without knowing they’re putting their kidneys at serious risk. This isn’t a rare side effect. It’s a predictable, dangerous, and often fatal interaction that doctors still miss. If you or someone you know takes lithium and uses over-the-counter painkillers regularly, you need to understand what’s really happening inside the body-and how to stay safe.
How Lithium and NSAIDs Collide in the Kidneys
Lithium works by stabilizing mood in bipolar disorder, but it’s a narrow therapeutic drug. That means the difference between a therapeutic dose and a toxic one is small. Your kidneys filter lithium out of your blood and into your urine. But when you take an NSAID-like ibuprofen, naproxen, or celecoxib-something unexpected happens. These drugs block enzymes called COX-1 and COX-2, which are responsible for making prostaglandins. Prostaglandins help keep blood flowing to your kidneys. When they’re suppressed, your kidneys get less blood. That slows down how fast lithium gets cleared from your body.That slowdown isn’t minor. Studies show lithium levels can jump by 25% to 60% within just 48 hours of starting an NSAID. A 2013 study in the Journal of Clinical Psychopharmacology found that even a single dose of indomethacin could cause lithium to build up to dangerous levels. The result? Toxicity. Symptoms like hand tremors, confusion, slurred speech, nausea, and even seizures can appear quickly. In severe cases, kidney damage becomes permanent.
Not All NSAIDs Are Created Equal
You might think, "I just take Advil once in a while-it can’t be that bad." But the risk isn’t the same across all NSAIDs. Indomethacin is the worst offender, increasing lithium levels by up to 60%. Piroxicam and naproxen follow closely behind, with 25-35% increases. Ibuprofen, the most common OTC painkiller, still raises lithium by 20-30%. Even celecoxib, marketed as a "kidney-friendly" NSAID, can push lithium levels up by 10-15% in people with existing kidney issues.Aspirin is the exception. It causes almost no change in lithium levels. But here’s the catch: aspirin isn’t typically used for chronic pain. If you’re taking daily pain relief, you’re probably not on aspirin. And even if you are, it’s not a safe long-term substitute-it carries its own risks, like stomach bleeding.
The real danger isn’t just the drug itself-it’s how often this combo slips through the cracks. A 2023 study in Health Affairs found that only 58% of primary care doctors knew NSAIDs were dangerous with lithium. That means if you go to your orthopedist for back pain or your dentist for a toothache, they may not even ask if you’re on lithium. And if they don’t ask, they won’t warn you.
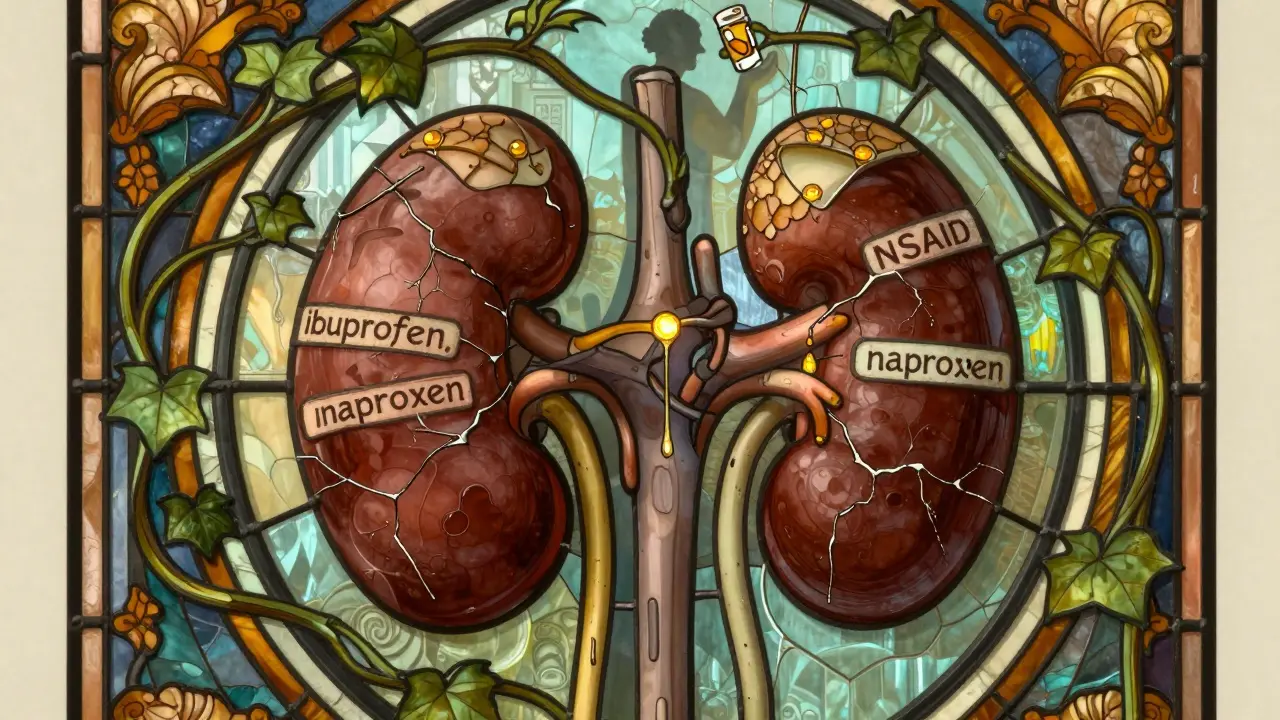
Why Kidneys Are the First to Fail
Lithium doesn’t just sit in your blood-it directly damages kidney cells. It interferes with a protein called GSK-3β, which leads to toxic buildup in the cells that filter urine. At the same time, NSAIDs reduce blood flow to the kidneys. So you’ve got two hits: one from the drug, one from the reduced circulation. Together, they create a perfect storm for acute kidney injury.A 2023 JAMA Network Open study tracked over 12,000 patients and found that those taking both lithium and NSAIDs had a 3.2 times higher risk of acute kidney injury compared to those on lithium alone. The highest risk? The first 30 days after starting the NSAID. That’s when lithium levels spike fastest.
For people over 65, the risk is even worse. Aging kidneys naturally filter slower. Combine that with lithium and an NSAID, and you’re looking at a 52% higher chance of hospitalization for kidney failure, according to data presented at the 2023 American Society of Nephrology meeting. One patient in a 2022 case series developed permanent kidney damage after just two weeks of taking ibuprofen for arthritis. His eGFR dropped by 40%-and never recovered.

What You Should Take Instead
The good news? There are safer options.Acetaminophen (Tylenol) is the first-line choice. It doesn’t affect kidney blood flow or lithium clearance. Studies show it causes less than a 5% change in lithium levels. But don’t overdo it-stick to 3,000 mg per day max to avoid liver damage. If you’re on multiple medications or drink alcohol, talk to your doctor about lowering that dose.
Tramadol is a second-line option for moderate to severe pain. It’s an opioid-like drug that doesn’t impact prostaglandins. It can slightly raise lithium levels (10-15%), but not nearly as much as NSAIDs. Start low-25 mg once daily-and increase slowly under supervision.
For chronic pain, physical therapy, heat therapy, or even low-dose antidepressants like duloxetine (Cymbalta) can help without touching your kidneys. If you’re on lithium for bipolar disorder, your mood stability matters more than your pain relief. Don’t sacrifice one for the other.
What to Do If You’ve Already Taken NSAIDs
If you’ve taken ibuprofen, naproxen, or any NSAID while on lithium, don’t panic-but act fast.- Stop the NSAID immediately.
- Call your psychiatrist or primary care provider. Tell them exactly what you took and when.
- Get a blood test for lithium levels within 24-48 hours.
- Drink plenty of water-3 liters a day-to help flush out excess lithium.
- Do not restart the NSAID without explicit approval from your care team.
Even after you stop the NSAID, the risk doesn’t vanish. Prostaglandin suppression can last 7-10 days. That means lithium levels may still be climbing. Your doctor should check your levels again at day 7 and again at day 14. Don’t assume you’re safe just because you stopped the pill.
Systemic Failures in Healthcare
This isn’t just about individual mistakes. It’s a broken system.Electronic health records have alerts for lithium and NSAIDs-but they only reduce co-prescribing by 35%. Why? Because many are soft alerts. Doctors can click "override" without entering a reason. In one study, 32% of lithium users still got NSAID prescriptions. That’s over 1 in 3.
Worse, many patients are prescribed NSAIDs by specialists who don’t know they’re on lithium. A 2023 study found that 41% of lithium toxicity cases came from non-psychiatrist prescribers who never checked the patient’s medication list. If you’re seeing multiple doctors, make sure each one knows you’re on lithium. Keep a printed list in your wallet or phone. Say it out loud: "I’m on lithium. Don’t give me any NSAIDs."
Health systems are trying to fix this. Kaiser Permanente cut co-prescribing from 32% to 12% by making alerts mandatory and adding provider education. The Veterans Health Administration? Only dropped from 30% to 25%. Progress is slow-and uneven.
What’s Being Done to Fix This?
The FDA updated lithium’s prescribing label in 2021 to include a boxed warning-the strongest type-for NSAID interactions. The European Medicines Agency now recommends hard stops in e-prescribing systems: if you’re on lithium, the system should block NSAID prescriptions unless a nephrologist approves it.There’s also new research. A 2023 clinical trial tested a prostaglandin E1 analog designed to protect kidney blood flow during NSAID use without affecting lithium clearance. Early results showed an 87% reduction in lithium level spikes. It’s still experimental, but it’s a sign that the medical community is finally taking this seriously.
Meanwhile, doctors are looking at alternatives to lithium itself. Drugs like valproate and lamotrigine don’t carry the same kidney risk. But here’s the catch: lithium is still the most effective drug for preventing suicide in bipolar disorder. A 2022 meta-analysis found it reduces suicide risk by 44%, compared to just 22% for other mood stabilizers. That’s why so many people stay on it-even as their kidneys weaken.
Final Advice: Protect Yourself
If you’re on lithium:- Never take an NSAID without talking to your psychiatrist first.
- Keep a list of all your medications and show it to every new doctor.
- Use acetaminophen for pain-stick to 3,000 mg/day.
- Drink 2.5-3 liters of water daily, especially if you’re over 60.
- Get your lithium levels checked every 3-6 months, and always after starting any new medication.
- Know the signs of toxicity: tremors, confusion, vomiting, dizziness, muscle weakness.
If you’re a doctor prescribing pain meds:
- Always check for lithium before prescribing NSAIDs.
- Make acetaminophen your default recommendation.
- Document your reasoning if you prescribe an NSAID anyway.
- Monitor lithium levels at day 3 and day 7 after starting the NSAID.
This interaction kills. It doesn’t happen by accident. It happens because we assume someone else is watching. Don’t assume. Ask. Check. Verify. Your kidneys-and your life-depend on it.
Can I take ibuprofen with lithium if I only use it once in a while?
No. Even a single dose of ibuprofen can raise lithium levels enough to cause toxicity. The risk isn’t about frequency-it’s about how your kidneys respond. Lithium clearance drops within 24-48 hours of taking an NSAID, and the effect lasts up to 10 days. There’s no safe "occasional" use when lithium is involved.
What are the early signs of lithium toxicity?
Early signs include fine hand tremors, increased thirst, frequent urination, nausea, mild confusion, and muscle weakness. These can be mistaken for side effects of lithium alone-but if they suddenly worsen after starting an NSAID, it’s a red flag. More severe symptoms include slurred speech, dizziness, seizures, and loss of coordination. If you notice any of these, stop the NSAID and get a blood test immediately.
Is Tylenol (acetaminophen) completely safe with lithium?
Yes, acetaminophen is the safest pain reliever for people on lithium. It doesn’t affect kidney blood flow or lithium clearance. However, you should still limit your daily dose to 3,000 mg or less to avoid liver damage, especially if you drink alcohol or have liver disease. Always check with your doctor before starting any new medication, even OTC ones.
How long does it take for lithium levels to return to normal after stopping an NSAID?
It can take 7 to 10 days for lithium levels to fully stabilize after stopping an NSAID. That’s because the drug’s effect on kidney blood flow lingers. Even if you feel fine, your lithium levels may still be elevated. Your doctor should check your levels at day 7 and again at day 14 to make sure they’ve returned to your target range.
Why do some doctors still prescribe NSAIDs to lithium users?
Many doctors simply don’t know the risk-or they underestimate it. A 2023 survey found that only 58% of primary care providers correctly identified NSAIDs as dangerous with lithium. Others assume the patient already knows, or they think "it’s just a little pain." But the data is clear: this interaction causes hospitalizations, permanent kidney damage, and death. It’s not a guess-it’s a proven danger that’s been documented for decades.
Should I switch from lithium to another mood stabilizer to avoid this risk?
That’s a decision you should make with your psychiatrist. Lithium is still the most effective drug for preventing suicide in bipolar disorder-cutting risk by 44%, compared to about 22% for alternatives like valproate or lamotrigine. While other mood stabilizers have fewer kidney risks, they may not work as well for you. If you’re doing well on lithium, the goal isn’t to stop it-it’s to manage your pain safely while staying on it.


Melissa Cogswell
January 30, 2026 AT 01:11I’ve been on lithium for 12 years and never realized how dangerous OTC painkillers could be. I used to pop ibuprofen like candy for my migraines. After reading this, I switched to Tylenol and started carrying a printed med list in my wallet. My last blood test showed my lithium levels are stable for the first time in years. Seriously, if you’re on lithium-stop guessing. Talk to your doctor. Your kidneys will thank you.
Also, if you’re a provider: make this a checklist. Don’t assume the patient knows. We don’t always remember what we’re on, especially when we’re in pain or depressed.
Diana Dougan
January 30, 2026 AT 05:25Wow. So let me get this straight-doctors are so dumb they don’t know ibuprofen + lithium = kidney death? And you’re shocked? Maybe stop prescribing lithium if it’s this fragile. Or better yet, stop letting people take OTC drugs without a PhD in pharmacology. I mean, I got my flu shot from a CVS clerk. Why should my meds be any different?
Bobbi Van Riet
January 31, 2026 AT 09:06This is such an important post. I work in a clinic and see this all the time. Patients come in with back pain, get prescribed naproxen, and two weeks later they’re in the ER with confusion and tremors. And the worst part? They don’t even realize lithium is the culprit because they think it’s just "side effects."
I now have a sticky note on my computer that says "CHECK LITHIUM BEFORE NSAID PRESCRIPTION" and I make every patient repeat back their meds. It’s annoying, yes-but it’s saved lives. I even printed out a one-page handout on lithium-safe pain relief and keep it on the counter. If you’re reading this and you’re on lithium-please, don’t be shy. Say it out loud: "I’m on lithium. No NSAIDs." Say it like you mean it. Because if you don’t, no one else will.
And for the love of God, drink water. Not just when you’re thirsty. Just drink. 3 liters a day. Your kidneys are working overtime already.
Holly Robin
February 1, 2026 AT 19:19THIS IS A BIG PHARMA COVER-UP. They don’t want you to know lithium is a slow poison. NSAIDs? They’re just the trigger. The real villain? The FDA. They knew about this for 40 years. Why did they only add a boxed warning in 2021? Because they were waiting for enough people to die. And now they’re pushing "alternatives" like valproate-guess what? That causes liver damage and pancreatitis. They’re just swapping one organ failure for another. They don’t care if you live or die-they care about profit. Your psychiatrist? They get kickbacks from pharma reps. Don’t trust them. Get your own blood tests. Buy a home lithium test kit. Fight back.
And if you’re still taking lithium? You’re being experimented on. Wake up.
Shubham Dixit
February 3, 2026 AT 06:45People in America are so weak. You can’t even take a painkiller without needing a medical degree? In India, we take aspirin with everything-fever, headache, joint pain-and we don’t die. Why? Because we don’t overthink. We don’t panic. We just take what works. Lithium? Fine. But stop acting like every pill is a nuclear bomb. Your body is not a lab. It’s a machine. It adapts. You’re just scared because you’ve been taught to fear medicine, not trust it. This post reads like fear porn. You’re scaring people for clicks. Real men don’t need acetaminophen to survive. They endure. Grow a spine.
KATHRYN JOHNSON
February 4, 2026 AT 06:50There is no excuse for this systemic failure. Every electronic health record in the U.S. should have a hard block on NSAID prescriptions for lithium patients. No override. No exceptions. This is not a suggestion. This is a matter of life and death. If your system allows a doctor to click "proceed" without a signed attestation, it is broken. And if your provider doesn’t proactively ask about lithium before prescribing any NSAID, they are negligent. Demand better. Document everything. And if you’re prescribed an NSAID while on lithium-report them. Immediately.
Blair Kelly
February 5, 2026 AT 02:49Let’s be real-this isn’t about kidneys. It’s about control. The medical industry wants you dependent. They want you scared. They want you to think you can’t take ibuprofen without a 30-minute consultation. But here’s the truth: you’re not fragile. You’re not broken. You’re just being manipulated into believing you need permission to feel better. Acetaminophen? Fine. But why is it the only option? Why not explore non-pharmaceutical solutions? Cold therapy. Stretching. Acupuncture? Why are we reducing pain to a pill? You don’t need to be a victim. You need to take back your agency. Stop asking for permission. Start asking for alternatives.
Lily Steele
February 5, 2026 AT 13:23Just wanted to say thank you for writing this. I’ve been on lithium since I was 19. I used to take ibuprofen for cramps and thought it was fine. I didn’t know until my mom had a near-death episode from this exact combo. Now I carry a card in my wallet that says "LITHIUM USER-NO NSAIDS." My doctor even gave me a bracelet. It’s embarrassing at first, but honestly? It’s saved me. If you’re reading this and you’re on lithium-do it. Don’t wait for a crisis. Just do it. And if someone asks why you have a bracelet? Tell them. They might not know either.
Also-Tylenol is your friend. I take 2,000 mg a day and feel fine. No drama. No panic. Just safety.
Gaurav Meena
February 6, 2026 AT 03:52Thank you for this life-saving post 🙏 I’m a nurse in Delhi and I’ve seen so many patients from the U.S. come in with lithium toxicity after taking Advil. It’s heartbreaking. Please, if you’re on lithium, treat this like a diabetic avoiding sugar. It’s not optional. It’s survival. And to all the doctors reading this: make this part of your intake checklist. Don’t wait for someone to die before you act. I’ve started handing out laminated cards to my patients with lithium-safe pain options. Simple. Clear. Life-saving.
You are not alone. You are not weak. You are strong for managing this. And you deserve to live without fear. Stay safe. Stay informed. And if you need someone to talk to-I’m here. 💙